Pericarditis: Symptoms, Causes, Diagnosis, Treatment, Complications
- Updated on: Jul 13, 2024
- 8 min Read
By
- Published on Oct 3, 2019
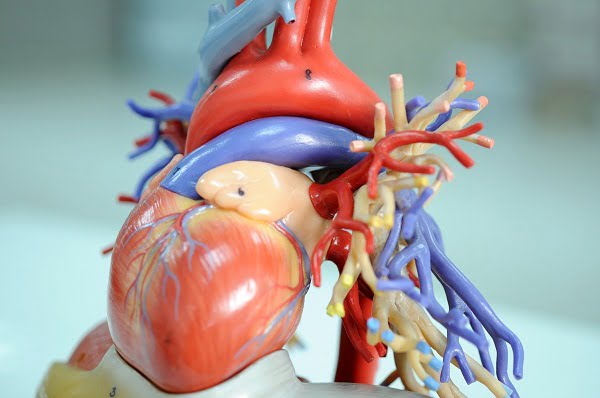
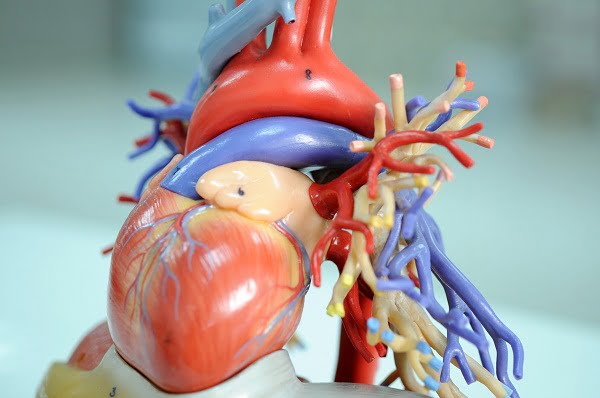
What is pericardium? What is pericarditis (inflammation around the heart)?
Pericarditis is an inflammation (swelling and irritation) of the pericardium or around the heart.
The pericardium is a two-layered thin sac that is filled with a fluid. It covers the outer surface of the heart and protects it. It also provides lubrication for the heart and shields it from any infection.
The two layers of the pericardium (inner and outer layer) can become inflamed if blood or fluid leaks between the two layers. The fluid keeps the layers from rubbing against each other and causing friction. In pericarditis, the inflamed tissue can rub against the heart. This makes the membrane around the heart red and swollen followed by a severe chest pain.
Pericarditis usually lasts for a short duration (10 days to 3 months) but sometimes attack can come and go for years. Pericarditis occurs because of following problems:
- Pericardial effusion – a condition of buildup of fluid in the pericardial sac
- Cardiac tamponade – a sudden pressure on the heart causing difficulty in pumping enough blood. This can be caused by the pericardial effusion when weight and pressure of the fluid buildup quickly.
- Constrictive pericarditis – a condition in which pericarditis comes back and becomes a longer-term problem. In such situations, the sac around the heart gets thick and stiff making it harder for the heart to pump blood.
What are the symptoms of pericarditis?
The symptoms of pericarditis include:
- Sharp chest pain (similar to a stabbing sensation) which may feel worse when swallowing and lying flat
- Neck pain extending across the shoulders and arms
- Fever and chills
- Sweating
- Nausea and dizziness
- Anxiety
- Lightheadedness
- Shortness of breath
- Heart palpitations
- Feeling sick, fatigue and weak
- Dry cough
- Abdominal or leg swelling
Who gets pericarditis?
Pericarditis can affect people of all ages. But it is more likely to develop in men 20 to 50 years old. 15 to 30 percent of patients with acute pericarditis may get it again and some of them eventually develop chronic pericarditis.
Pericarditis Causes: What causes pericarditis?
The cause of pericarditis is hard to determine. Mostly, the cause of pericarditis is unknown (idiopathic pericarditis) and sometimes, doctors suspect it as a viral infection. However, there are many causes of pericarditis which includes:
Infections
Some infections can cause pericarditis like:
- Viruses (like gastrointestinal)
- Bacteria (like tuberculosis)
- Fungal infection
- Infection from a parasite
- HIV (human immunodeficiency virus)
Inflammatory diseases
Generalized inflammation in other places within the body can also give rise to inflammation of the pericardium. Some examples of such inflammatory diseases include:
- Rheumatoid arthritis
- Inflammatory bowel disease
- Scleroderma
- Systemic lupus erythematosus (SLE)
- Ankylosing spondylitis
Metabolic illness
Metabolic-related pericarditis is caused by:
- Kidney failure
- Hypothyroidism
Heart disease
Heart attacks can results in irritation and inflammation of the lining of the pericardium. Open heart surgery sometimes also causes pericarditis.
Radiation
Radiation therapy used in cancer treatments can cause pericarditis as excessive use of radiation can injure the pericardium.
Cancerous tumors
When cancer spreads to the heart, it causes inflammation in the pericardium. Pericarditis occurs most commonly in breast cancers and lung cancers.
Trauma
Any trauma to the chest may become the causing factor of pericarditis. Injuries with a steering wheel (blunt injury) or with a bullet or knife (sharp injury) can cause the disease. Sometimes, invasive cardiac procedures and cardiopulmonary resuscitation (CPR) can cause trauma to the heart and induces pericarditis.
Drugs and toxins
A number of medications like procainamide, hydralazine, methyldopa, isoniazid, mesalazine, and reserpine can cause pericarditis.
What are the risk factors of pericarditis?
The risk of getting pericarditis become high after:
- A heart attack
- Heart surgery (postpericardiotomy syndrome)
- Radiation therapy
- Percutaneous treatment (like cardiac catheterization or radiofrequency ablation (RFA))
What are the different types of pericarditis?
Pericarditis is classified on the basis of symptoms and causes:
Pericarditis Based on Symptoms
Acute pericarditis
In acute pericarditis, chest pain develops suddenly (also affecting the neck, shoulders and back). Severe pain is felt during inspiration and while lying down, but pain decreases when one sits up.
The symptoms may last for ten days to three months. This type of pericarditis can be easily resolved in a few days with appropriate and timely treatment.
Acute pericarditis can be the result of viral/bacterial infection, metabolic disorders, cardiac arrest or a blunt injury or it can be without any symptoms (idiopathic).
Chronic pericarditis
When the condition persists over a period of time and the symptoms last longer than six months, it is chronic pericarditis. In this condition, the patient may or may not have the typical chest pain, but may experience other symptoms like tiredness, shortness of breath, and coughing.
Autoimmune disorders (where the antibodies produced by the body attack its own cells and tissues) such as lupus, scleroderma, and rheumatoid arthritis results in chronic pericarditis.
Recurrent pericarditis
Repeated episodes of pericarditis are referred to as recurrent pericarditis. It is a debilitating condition and has to be treated carefully and timely. Its treatment depends on the cause of the condition.
Pericarditis Based on Causes
Constrictive pericarditis
Thickening or scarring of the pericardial layers may start constricting the heart within the thoracic cavity. Thus limiting the effective functioning of the heart. Such condition is known as constrictive pericarditis.
Pericardial effusion
The pericardial cavity is filled with an approximately 20–50 ml of fluid. Sometimes, some medical conditions (such as kidney failure) or some invasive cardiac procedures may cause a gradual accumulation of fluid within the pericardial cavity. This accumulation may compress the surrounding structures like lungs and stomach. This condition is known as pericardial effusion and its symptoms include dyspnea, nausea and bloating.
Cardiac tamponade
Sometimes, the accumulation of fluid can be steady and the fluid volume can increase up to 80 to 200 ml. Such high levels of pericardial fluid volume can lead to pericardium malfunction and should be treated as an emergency.
Viral pericarditis
Coxsackieviruses, influenza virus, agents of viral enteritis, human immunodeficiency virus (HIV) and echovirus are the viruses that cause viral pericarditis. The most common symptom of this condition is infection in the upper airways.
Purulent pericarditis
Procedures including surgery in the chest region, immunosuppression and chemotherapy are the causes that can lead to this type of pericarditis.
Tuberculous pericarditis
Some patients having pulmonary tuberculosis may develop tuberculous pericarditis. HIV-positive patients are also at a greater risk of developing this type of condition.
Radiation Pericarditis
This type of pericarditis is caused due to radiation therapies done for the treatment of various diseases such as cancer. This condition can develop within weeks or months after the exposure.
Traumatic pericarditis
Any kind of trauma – sharp or blunt may cause traumatic pericarditis. Invasive cardiac procedures like cardiac diagnostic catheterization and electrophysiological ablation procedure may also give rise to such condition.
Malignancy
Malignancy pericarditis is mainly caused by metastatic disease in which the cells spread to new areas of the body. This condition is common in metastasized bronchogenic, Hodgkin’s disease and lymphoma.
How is pericarditis diagnosed?
The diagnosis of pericarditis is based on medical history, physical exam and the results from tests performed.
Medical History
For having an idea about the medical history of the patient, the doctor may ask whether the patient:
- Has had a recent respiratory infection
- Has had a recent heart disease or chest injury
- Has any other medical condition
The doctor may also ask about:
- Symptoms of the disease
- Description of the symptoms
- Location
- Severity while lying down, breathing or coughing
Physical Exam
The inflammation of the pericardium increases the amount of fluid between its two layers of tissue. In the physical exam, the doctor looks for signs of excess fluid in the chest. One of the common sign is the pericardial rub. This is the sound produced when the pericardium rubs against the outer layer of the heart. This sound can be listened by placing a stethoscope on the patient’s chest.
Diagnostic Tests
Some tests are prescribed to diagnose the condition and the severity. The most common tests are:
EKG (electrocardiogram)
This test detects the heart’s electrical activity and records it.
Chest x-ray
A chest x-ray creates pictures of heart, lungs and blood vessels. These pictures can show whether the patient has an enlarged heart which is a sign of excess fluid in the pericardium.
Echocardiography
This test also creates pictures using sounds. The pictures show if there is any irregularity in size and shape of the heart and also show the functioning of the heart. This test also shows whether fluid has built up in the pericardium.
Cardiac CT (computed tomography)
This is a type of x-ray that creates a detailed picture of your heart and pericardium. It is used to rule out other causes of chest pain.
Cardiac MRI (magnetic resonance imaging)
Detailed pictures of your organs and tissues are created with the help of powerful magnets and radio waves. Any changes in the pericardium can be easily detected using this test.
Blood tests
Blood tests are done to find out:
- Whether the patient had a heart attack
- How well the heart is working
- The cause of pericarditis
- How inflamed the pericardium is
Sedimentation rate (ESR) and ultrasensitive C reactive protein levels that are markers of inflammation are higher than normal if a person is having pericarditis.
Pericarditis Treatment: How is pericarditis treated?
The major goals of treating this condition include:
- Reduction of the inflammation of the pericardium
- Pain relief
- Finding and curing the root cause
- Ruling out further complications
Various treatment options that are used are given below:
Nonsteroidal Anti-Inflammatory Drugs
Severe pain along with fever is the main symptom of the disease. These medications are used to relieve the pain and resolve the inflammation that causes the fever.
Aspirin, ibuprofen, indomethacin, naproxen and ketorolac are some of the anti-inflammatory drugs used in the treatment. The patient is also advised to rest for about a week or two. This method promises recovery in 70–80% of the cases.
Colchicine
Colchicine is given to the patient suffering from acute or recurrent pericarditis. This medicine helps to reduce inflammation and the severity of symptoms.
It also decreases the risk of recurrence. Colchicine is often combined with Nonsteroidal anti-inflammatory drugs for better results.
Abdominal pain, vomiting and diarrhea are some of the side effects of this drug.
Corticosteroids
Systemic corticosteroid therapy is given to patients who have refractory symptoms. One example of corticosteroid is prednisone that is used most of the time. Corticosteroids drugs are useful in reducing pericardial inflammation as they block several immunological pathways.
Weight gain, mood swings and increased sweating are the side effects of these medicines if continued for long.
Surgical (Interventional) Therapies
Medications alone are not sufficient in some cases including pericardial effusion, cardiac tamponade, recurrent pericarditis and constrictive pericarditis. In such situations, some surgical intervention is needed as part of the treatment protocol.
Pericardiocentesis
Pericardiocentesis is the medical term for removal of fluid from the pericardium in order to relieve pericardial effusion and cardiac tamponade. This technique is also useful in reducing the pressure on the heart.
Side effects of pericardiocentesis include bleeding, infection and damage to the heart.
Pericardiectomy
This technique is used selectively and it involves surgical decompression of the pericardium. This can be achieved by routine heart surgery or by video-assisted thoracoscopy. This treatment method is used only when a patient has recurrent pericarditis or recurrent cardiac tamponade.
Other Techniques
Balloon pericardiotomy is a less invasive procedure and it is used in the treatment of patients who have reduced life expectancy. In this technique, a balloon catheter is inserted into the pericardial space.
What are the complications related to pericarditis?
The complications of pericarditis may include:
Constrictive Pericarditis
Long-term inflammation and chronic recurrences of the disease can develop permanent thickening and contraction of the pericardium. This results in a rigid pericardium that has lost its elasticity.
Rigid pericardium makes it difficult for the heart to function properly. This condition is called constrictive pericarditis. The main symptoms of this condition are severe swelling of the legs and abdomen and shortness of breath.
Cardiac tamponade
Cardiac tamponade is a dangerous condition and it occurs when too much fluid collects in the pericardium. Excess fluid puts pressure on the heart. Thus the heart does not fill properly and less blood leaves the heart. This causes a significant and dramatic drop in blood pressure. This condition can be very dangerous if not treated at time.
The risk of the long-term complications can be greatly reduced if pericarditis is diagnosed early and treated properly.
Pericarditis Prevention: Can pericarditis be prevented?
Acute pericarditis cannot be prevented. However, recurrent acute episodes, complications of the disease and chronic pericarditis can be prevented if correct measures are taken.
The prevention steps include:
- Getting prompt treatment
- Following the treatment plan
- Getting ongoing medical care as advised by the doctor.