How to Balance a Diabetic Diet With Genetic Insights
- Updated on: Dec 17, 2024
- 4 min Read
- Published on Dec 17, 2024
Balancing a diabetic diet with genetic insights involves creating a nutrition plan tailored to individual genetic predispositions. This personalized approach enhances blood sugar management and reduces the risk of complications associated with diabetes. This article will explore how genetics influence diabetes and how you can incorporate these insights into your daily eating habits.
Understanding the connection between genetics and diabetes is essential for effectively balancing your diet. This foundational knowledge will help you make informed dietary decisions, aligning your eating habits with your unique biological needs.
What Role Do Genes Play in Diabetes?
Genes influence how your body processes essential nutrients, including carbohydrates, fats, and proteins. Specific genetic variations can increase your risk of developing type 2 diabetes by affecting insulin production, insulin sensitivity, or glucose metabolism. For instance, the TCF7L2 gene, often associated with diabetes, impacts how your body responds to glucose and regulates insulin secretion.
Understanding these genetic factors helps you identify your susceptibility to certain dietary triggers that can worsen blood sugar control. By addressing these predispositions, you can make proactive changes to stabilize blood sugar levels. For example, someone with a genetic tendency toward insulin resistance might benefit from reducing simple carbohydrates in their diet while increasing fiber and protein intake.
Gene-Diet Interactions and Their Impact on Diabetes
Diet and genetics are deeply interconnected. Gene-diet interactions, also known as nutrigenomics, explore how specific foods or nutrients influence your body based on your genetic profile.
For instance, genetic variations can affect how your body metabolizes certain types of carbohydrates or fats. These variations may lead to either efficient or inefficient nutrient processing, impacting your blood sugar levels.
- For example, some individuals with genetic markers related to lipid metabolism might benefit from incorporating more omega-3 fatty acids to support heart and metabolic health.
- Conversely, those sensitive to dietary sugars may need to strictly monitor their intake of high-glycemic-index foods like white bread or sugary beverages.
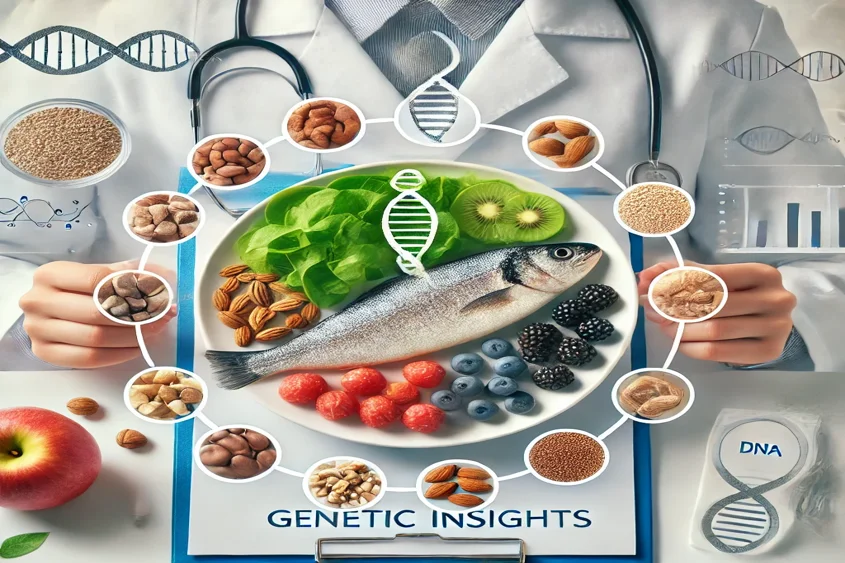
By aligning your diet with these genetic insights, you can create a targeted nutritional plan that minimizes the impact of diabetes-related complications.
Personalized Nutrition for Diabetes Management
After gaining a deeper understanding of the genetic factors influencing your health, the next step is implementing these insights into a personalized nutrition plan. This approach ensures your dietary choices are tailored to support your blood sugar stability and overall well-being.
The Role of Genetic Testing
Genetic testing is a powerful tool that provides insights into your unique nutritional needs and predispositions. These tests analyze your DNA for specific markers linked to diabetes risk, nutrient metabolism, and other health factors.
By identifying genetic variations, healthcare professionals can create tailored dietary strategies that align with your body’s needs.
For example, a genetic test may reveal a predisposition to higher triglyceride levels in response to saturated fats.
Armed with this knowledge, you can focus on healthier fat sources like avocados, nuts, and olive oil instead of butter or red meat. Similarly, genetic markers for impaired glucose metabolism might prompt you to limit sugary and starchy foods in favor of whole grains and leafy greens.
Genetic testing is not a one-time solution but an ongoing process. As your health evolves, these insights can be updated and refined, ensuring your diet effectively manages your condition.
Personalized Dietary Recommendations
Using genetic insights, dietary recommendations become more precise and actionable. Instead of following generalized dietary advice, you can make targeted adjustments to your macronutrient ratios, food choices, and portion sizes. This tailored approach ensures that your diet harmonizes with your body’s unique needs.
For example:
- Carbohydrate Sensitivity: If genetic testing shows a high carbohydrate sensitivity, consider adopting a low-glycemic diet. Replace white rice and refined pasta with quinoa, brown rice, or lentils to stabilize blood sugar levels.
- Fat Metabolism: If your genes suggest difficulty metabolizing saturated fats, focus on plant-based fats such as seeds, nuts, and olive oil to support heart health and reduce inflammation.
- Protein Needs: For individuals predisposed to muscle loss or poor protein utilization, increasing lean protein sources like chicken, tofu, or fish can enhance blood sugar regulation and overall metabolic health.
Transitioning to a personalized diet might initially feel overwhelming, but with proper guidance, these changes can become a sustainable part of your lifestyle.
Practical Steps to Balance Your Diet Using Genetic Insights
After understanding how genetics influence your dietary needs, it’s essential to translate this knowledge into actionable steps. Here’s how to incorporate genetic insights into your daily routine to improve blood sugar management and overall health.
Incorporate Nutrient-Dense Foods
Nutrient-dense foods are the cornerstone of any healthy diet, especially when managing diabetes.
Focus on whole foods that provide essential vitamins, minerals, and antioxidants without spiking blood sugar levels. Examples include:
- Vegetables: Leafy greens like spinach and kale, cruciferous vegetables like broccoli and cauliflower, and non-starchy vegetables such as zucchini and bell peppers.
- Proteins: Lean sources like chicken, fish, beans, lentils, and tofu help regulate blood sugar and maintain muscle mass.
- Healthy Fats: Incorporate avocado, nuts, seeds, and olive oil to improve heart health and provide sustained energy.
Pairing these nutrient-dense foods with genetic insights ensures you meet your dietary needs while managing your diabetes effectively. Additionally, creating a diabetic diet plan to lose weight tailored to your genetic profile can provide more targeted solutions for maintaining blood sugar control and achieving a healthy weight.
Combining these approaches allows you to optimize your diet to better align with your body’s unique requirements. Let me know if this works or requires further refinement!
Monitor Blood Sugar Responses
Even with a personalized diet, monitoring your blood sugar levels is crucial. This practice allows you to understand how your body responds to different meals and make adjustments as needed. For example:
- Test blood sugar levels two hours after eating to track post-meal spikes.
- Maintain a food diary to identify patterns between certain foods and blood sugar fluctuations.
Over time, this process helps refine your diet, ensuring it remains effective and aligned with your genetic insights.
Final Note
Balancing a diabetic diet with genetic insights is an innovative and effective strategy to manage blood sugar levels and improve overall health.
Understanding the relationship between your genes and dietary needs allows you to create a nutrition plan that works for your unique biology. With the right tools, consistent monitoring, and support from healthcare professionals, you can confidently take control of your diabetes management and achieve a healthier lifestyle.