About Cervical Cancer (Overview and Types): Causes, Symptoms, Signs, Diagnosis, Treatment, Prevention
- Updated on: Jul 23, 2024
- 17 min Read
- Published on Mar 16, 2018
What Is Cervical Cancer?
Cancer begins when cells in our body begin to grow in an uncontrolled manner. Cells in any part of the body can become cancerous, and can spread to other areas of the body too.
Cervical cancer is a type of cancer that begins in the cells lining of the cervix. According to the American Cancer Society, about 12,280 diagnoses of cervical cancer were estimated to be made by the end of 2017 in the United States. More than 4,000 women in the U.S. were estimated to die from this type of cancer in that year.
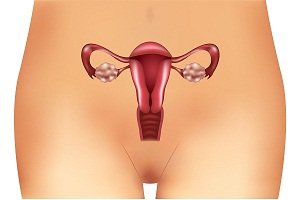
What is cervix?
Cervix is the lower part of the uterus (womb). The fetus grows in the body of the uterus. The cervix connects the body of the uterus to the vaginal canal also called the birth canal. The cervix leads from the uterus to the vagina (birth canal).
The cervix has two different parts and is covered with two different types of cells.
- The part of the cervix closest to the body of the uterus is called the endocervix. It is covered with glandular cells.
- The part close to the vagina is called the exocervix (or ectocervix). It is covered with squamous cells.
The two types of the cell of cervix in two different regions meet at the transformation zone. The exact location of the transformation zone changes with age and as a woman gives birth. Most cervical cancers begin in the cells in this transformation zone.
Abnormal cells in the cervix can become cancer
Cervical cancer starts when healthy cells on the surface of the cervix change and grow in an uncontrolled way, thereby forming a mass called a tumor. A tumor is not always cancerous. It can be cancerous or benign. A cancerous tumor is malignant, which means it can spread to other tissues or parts of your body. A benign tumor means that the tumor will not spread.
In the beginning, the changes in a cell are abnormal, and not cancerous. Scientists say that, however, some of these abnormal changes are the starting point of cancer. Some abnormal cells can go away without any treatment, but others can become cancerous. This state of the cancer is called dysplasia.
The abnormal cells, also sometimes termed as precancerous tissues, need to be removed to keep cancer from progressing further. The precancerous tissue in the cervix can be removed without harming your healthy tissue, but sometimes, a hysterectomy is required to prevent cervical cancer. Hysterectomy involves removal of the entire uterus and cervix.
Treatment of these precancerous cells or lesions depends on the following factors:
- Size of the lesion
- Type of changes that have happened in the pre-cancerous cells
- Whether the woman wants to have children in future
- Woman’s age
- General health of the woman
- Personal preference of the woman
When the precancerous cells and lesions change into cancer cells and spread into the cervix or to other organs of the body, the cancer is called cervical cancer.
Types of cervical cancer
Cervical cancers and cervical pre-cancers are generally categorized based on how they appear when viewing under a microscope.
There are three main types of cervical cancer – squamous cell carcinoma, adenocarcinoma, mixed carcinomas. Squamous cell carcinoma begins in the thin, flat cells that line the cervix. Adenocarcinoma begins in cervical cells that make mucus and other fluids.
Squamous cell carcinomas
Most cervical cancers are squamous cell carcinomas. These cancers develop from cells in the exocervix. Squamous cell carcinomas most often begin in the transformation zone.
Adenocarcinoma
Cervical adenocarcinoma develops from the mucus-producing gland cells of the endocervix. These tyupes of cancers have become more common in the past 30 years.
Adenosquamous carcinomas or mixed carcinomas
Some types of cervical cancers may have features of both squamous cell carcinomas and adenocarcinomas. These are called adenosquamous carcinomas or mixed carcinomas. They are not very common though.
Other rare types of cervical cancers
Almost all of the cervical cancer cancers are either squamous cell carcinomas or adenocarcinomas, but there are some other rare types of cervical cancers also that can develop in the cervix. These other rarer types are:
- Melanoma
- Sarcoma
- Lymphoma
These cancers rarely develop in the cervix, but are more common in other parts of the body.
Cervical Cancer: Key Statistics and Facts
In year 2017, more than 12,000 women in the United States were diagnosed with cervical cancer. It is estimated that more than 4,000 deaths occurred from the disease this year.
The American Cancer Society’s estimates for cervical cancer in the United States for year 2018 are as follows:
- More than 13,000 new cases of invasive cervical cancer will be diagnosed
- More than 4,000 women will die from cervical cancer
In the past, cervical cancer was once one of the most common causes of cancer death for American women. The cervical cancer death rate reduced significantly with the increased use of the Pap test. Pap test can help in screening of the cervical cancer and can find changes in the cervix before the actual cancer develops. Pap test can also detect cancer at an early stage when it’s small and easier to cure. However, the decrease in death rate has not reduced much further in the last one and a half decade.
Do we know what causes cervical cancer?
There has been a lot of research on understanding the mechanisms of cervical cancer and what happens in the cells of the cervix when cancer develops there. Accordingly, several risk factors have been defined that increase the chances of a woman to develop cervical cancer. These are listed and discussed later in the article.
DNA is the chemical in our cells that form our genes. Genes then control the functioning of our cells. DNA can affect us in many ways. Cancers can be caused by DNA mutations (gene defects) that turn on oncogenes or turn off tumor suppressor genes. This can have an effect on the progression and spread of the cervical cancer.
How do women get cervical cancer? What causes cervical cancer?
Almost all cervical cancers are caused by continued infection with one of the HPVs (Human papilloma viruses). Most people with HPV infection do not develop cancer. HPVs group constitute more than 100 types of viruses and only few types of them are associated with cervical cancers. Other HPV types cause diseases such as warts on the skin or genitals. HPVs can also cause cancers of the male genital organs, and cancers of mouth, throat, and anus in both sexes.
The HPV infection is spread through sexual contact or skin-to-skin contact. The infection generally goes away on its own. But, in some women, the infection may continue for a longer time and can cause pre-cancerous changes in the cells of the cervix. There are tests (pap screening tests) to detect these changes.
But it must be understood that HPV is not the only cause of cervical cancer. There are other risk factors too of cervical cancer such as smoking and HIV infection etc.
The cervix contains two types of cells:
- the lining cells of the outer cervix, known as squamous cells
- the cells that line the interior channel of the cervix
The point at which the squamous and glandular cells meet is known as the transition zone. Most cervical precancers and cancers begin to grow in this zone only. About 90% of cervical cancers originate from the squamous cells. These are called squamous cell carcinomas.
Cervical cancer prevention: Can you prevent cervical cancer?
The most common form of cervical cancer starts with pre-cancerous changes. With extensive research on this type of cancer in the last decades, scientists have developed ways to stop or slow down the disease from developing or progressing.
The first way to prevent a cervical cancer is to find and treat pre-cancers before they become actual cancers.
How to detect cervical pre-cancers?
Usually two tests are done for detecting cervical pre-cancers:
- testing (screening) to find pre-cancers before they can turn into invasive cancer through a Pap test (also called Pap smear)
- human papillomavirus (HPV) test
If a pre-cancer is found in the above tests, it can be treated and stopped before the actual cervical cancer starts to develop and spread. According to a study, it was found that most invasive cervical cancers are found in women who never had regular Pap tests.
The Pap test is a diagnostic method for detecting cervical cancer and other types of cancers of female reproductive systems such as endometrial cancer, uterine cancer etc. It is used to collect cells from the cervix, which are then examined under a microscope to find cancer and pre-cancer cells. A Pap test can be done by a gynecologist during a pelvic exam.
What can you do to prevent pre-cancers before they convert to cervical cancers?
Here is a list of things you can to for preventing cervical pre-cancers:
- Ensure an HPV vaccination is done
- Regular testing for HPV viruses
- Quit smoking and use of tobacco
- Use condom as the HPV viruses can pass through sex
Read more about Cervical Cancer Prevention and Early Detection.
What are the risk factors for cervical cancer?
There are several risk factors that can increase your chance of developing cervical cancer. If you do not have any of these risk factors, the chances that you develop cervical cancer are very low.
While the risk factors for any cancer increase the chances of developing that cancer, this does not mean one would always it. Similarly, having no risk factors does not mean that the person will never get the cervical cancer or any other cancer. When a woman develops cervical cancer, it might not be possible to say with surety that a particular risk factor triggered it.
Who develops cervical cancer?
Cervical cancer generally occurs in midlife and is most frequently diagnosed in women between the ages of 35 and 45. It rarely develops in women younger than 20 years in age. About 15% of cases of cervical cancer are found in women over 65 years. However, these cancers rarely occur in women who have got regular screening tests for cervical cancer before the age of 65.
Hispanic women are more likely to get this type of cancer, followed by African-Americans, Asians and Pacific Islanders, and whites. American Indians and Alaskan people have the lowest risk of developing cervical cancer in the United States.
Common cervical cancer risk factors are:
- Tobacco use or smoking
- Being overweight
- Long-term use of oral contraceptives
- Having three or more full-term pregnancies
- Having a first full-term pregnancy at an early age of below 16 years
- HIV infection
- Immune system suppression
- HPV infection
- Chlamydia infection in the past
- Family history of cervical cancer
- Economic status (Poverty)
- Herpes
- Use of intrauterine devices (IUD)
- Herpes
Some of these cervical cancer risk factors are discussed below.
Human papillomavirus (HPV) infection
Human papillomavirus (HPV) infection is the most important risk factor for cervical cancer. HPV constitute more than 150 related viruses. Some of them cause warts, which is a common problem. Not all of them cause cancer. The HPV types that are most commonly associated with cervical cancer are HPV16 and HPV18.
Some types of HPV may cause warts around the genital organs and in the anal area in both males and females. But they generally are not associated with cervical cancer.
According to various studies, the infection with this virus is a common risk factor for cervical cancer. Sexual activity with someone who has HPV can cause a person to get HPV virus.
Smoking and tobacco use
Smoking causes exposure to many cancer-causing chemicals that affect several organs of a person. Not only active but passive smoking is also harmful. These harmful substances are absorbed through the lungs and are carried throughout the body through the bloodstream.
The dangers of smoking are more in women as compared to risks in men. Women who smoke are about twice as likely as non-smokers to get cervical cancer.
Researchers have found tobacco by-products in the cervical mucus of women who smoke. These substances are thought to damage the DNA of cervix cells leading to cervical cancer.
Chlamydia infection
Chlamydia is bacteria that can spread by sexual contact and cause infection of the reproductive organs. It can even lead to infertility in women. Some studies show a higher risk of cervical cancer in women who have or had it in the past.
Chlamydia infection does not generally cause any symptoms of the infection. It is usually diagnosed when tests are done for some other condition. Read more about Chlamydia infection.
Obesity and diet
Women who do not consume enough fruits and vegetables may be at high risk for cervical cancer. A low fiber and high fat diet can also cause obesity, which is another risk factor for cervical cancer.
Overweight women are more likely to develop adenocarcinoma in the cervix.
Long-term use of oral contraceptives (birth control pills)
Recent research shows that oral contraceptives may be linked to an increased risk of cervical cancer. But more research is required to understand how oral contraceptive lead to the development of cervical cancer in women.
Weak immune system
Our immune system plays an important role in destroying the cancer cells and reducing their growth rate and spread in the body. Women with HIV have a weakened immune system. They are at an increased risk of getting cervical cancer.
Women who take drugs to suppress their immune systems, such as during the treatment of certain autoimmune diseases or those who consumed such drugs while they had an organ transplant are also at high risk of the cervical cancer.
Use of intrauterine devices (IUD)
Some research studies indicate that women who had ever used an intrauterine device had a lower risk of cervical cancer. The protective effect remained even after the IUDs were removed.
Using an IUD might also lower the risk of endometrial (uterine) cancer. However, IUDs can have some other risks. You should first discuss with your doctor if you want to use an IUD.
Several full-term pregnancies
Women who have had 3 or more full-term pregnancies are at an increased risk of developing cervical cancer. Researchers say that hormonal changes during pregnancy may be a reason for this. Another reason that scientists suggest could lead to higher risk is that pregnant women have weaker immune systems. This can cause the infections and cancer growth to grow in their bodies.
First pregnancy at an early age of less than 17 years
Women with age lesser than 17 years at the time of their first pregnancy are more likely to get cervical cancer later in their lives. They are about 2 times more likely to get cervical cancer in future than women who had first pregnancy at 25 or more years of age.
Economic status and other socioeconomic factors (Poverty)
Cervical cancer is more common among groups of women who do not have access to screening for cervical cancer. These are more likely to include black women, Hispanic women, and American Indian women, poor women.
Genetics: family history of cervical cancer
Cervical cancer can run in families. If your mother or sister had cervical cancer, your chances of getting it are higher than others who do not have the disease in their family.
Research shows that this tendency of genetic linkages may be caused by an inherited disorder that makes some women less able to fight HPV infection than others.
Exposure to diethylstilbestrol (DES)
Children of women who take this drug during pregnancy to prevent miscarriage have an increased risk of developing a rare type of cancer of the cervix or vagina. Women who are exposed to diethylstilbestrol must consider a routine annual pelvic examination. Doctors will take samples of their cells from all sides of the vagina to check for abnormal cell growth or any other abnormality.
DES-related clear cell adenocarcinoma is more common in the vagina than the cervix. The risk is greatest in women whose mothers took the drug during their first 16 weeks of pregnancy. The average age in which a woman gets DES-related clear-cell adenocarcinoma is 19 years, according to American Cancer Society.
Signs and symptoms of cervical cancer
Generally, pre-cancerous changes in the cervical cells and early cancers of the cervix do not cause any visible signs and symptoms. Therefore, a regular screening for the cervical cancer is done through Pap and HPV tests to detect pre-cancers early and prevent the development of cervical cancer. This is discussed above.
Common signs and symptoms of advanced cervical cancer may include abnormal or irregular vaginal bleeding, pain during sexual intercourse, abnormal vaginal discharge with a foul smell etc.
When should you contact a doctor?
Consult a doctor if you note these signs and symptoms of cervical cancer. Having these systems does not mean you will certainly have cervical cancer. These symptoms could also be signs of other health problems, not related to cervical cancer.
- Bleeding between regular menstrual periods
- Bleeding after a pelvic examination
- Bleeding after menopause
- Bleeding after sexual intercourse
- Bleeding after douching
- Heavy or unusual discharge that may be watery, thick, and possibly have a smell
- Frequently urinating
- Pelvic pain not related to your menstrual cycle
- Pain during urination
- Vaginal odor, unpleasant smelling vaginal discharge
Other symptoms when the cervical cancer is advanced
If the cancer spreads out of the cervix and into nearby tissue and organs, it can cause many other symptoms, such as:
- Constipation
- Severe pain in your side or back due to swelling in the kidneys. This is due to a condition called hydronephrosis.
- Weight loss
- Changes to your urinary and bowel habits
- Loss of appetite
- Blood in your urine (haematuria)
- loss of bladder control (urinary incontinence)
- Pain in bones
- Swelling of the legs
- Extreme fatigue
Diagnosis of cervical cancer: What are the tests and procedures to diagnose cervical cancer?
There are many tests to find, or diagnose, cervical cancer. Some tests are done to understand if the cervical cancer has spread to another part of the body from where it originally started and to what extent. Such a cancer that has spread to other locations is called metastatic cancer and the process is called metastasis.
There are several types of imaging tests that can show if the cancer has spread and to what extent. These tests can show pictures of the inside of the body. Healthcare practitioners use these tests to understand the stage of a cancer and define the treatment plan accordingly.
Commonly used tests for the diagnosis of cervical cancer and learning the spread of the cervical cancer to other locations
The list below describes options for cervical cancer diagnosis. But not all of these tests will be done for every person. These tests may be helpful for your doctor to decide about the treatment of your cancer. Your doctor will recommend which tests you need based on several factors such as the following.
- Type of your cancer
- Stage of the cancer
- Signs and symptoms
- Your age
- Your medical condition and health
- Results from earlier medical tests
These tests can be recommended by your doctor for cervical cancer diagnosis.
Medical history and physical exam
Your doctor will first ask you questions about your personal and family medical history. He or she may ask about information such as the various risk factors and symptoms of cervical cancer in your case.
A complete physical examination will be done to help evaluate your general state of health. Your lymph nodes will be felt for evidence of metastasis (cancer spread).
Pelvic examination
The doctor tries to feel a woman’s uterus, vagina, ovaries, cervix, bladder, and rectum to check for any abnormalities. A Pap test is often done at the same time. The doctor may use a speculum to insert into the vagina for better visualization and tissue extraction.
Pap test
It is also called a smear test. In a Pap smear test, your doctor will gently scrape the outside of the cervix and vagina to take some samples of the cells for investigation.
Traditional Pap methods were hard to read because cells were covered with mucus or blood. Improved Pap tests are now available for better diagnosis, such as these:
Liquid-based cytology test: This test is also called ThinPrep or SurePath. It allows transfer of a thin layer of cells to a test slide after removing the blood or mucus from the sample taken from the body. The sample can be preserved and used later along with other tests such as the HPV test at the same time.
Computer screening: This test is also called AutoPap or FocalPoint test. It uses a computer to scan the sample extracted from the body for finding and examining the abnormalities.
HPV typing
HPV test is similar to a Pap test. The doctor may test for HPV at the same time as a Pap test or after Pap test results show any suspected cancer cells in the cervix.
Strains of HPV (HPV-16 and HPV-18) are usually detected in women with cervical cancer which helps confirm the cervical cancer diagnosis. If the HPV test is positive, this means the test found the presence of HPV. But this does not the woman will always have cervical cancer. Many women have HPV but do not have cervical cancer. HPV testing alone is not a conclusive test for cervical cancer.
If both the Pap test and HPV testing showed some abnormal cells and abnormalities, your doctor may order one or more of these diagnostic tests:
Colposcopy
If abnormal cells are found on the Pap smear, a colposcopy procedure is then performed.
You will be asked to lie on the exam table as you do with a pelvic exam. A speculum will be placed in the vagina to help the doctor see your cervix.
Colposcopy uses a microscope with a small lighted lamp in it to investigate the external surface of the cervix during a pelvic examination. If the doctor finds any abnormal cells in the examined site, a small tissue sample is taken for examination by a pathologist through a biopsy procedure to look for pre-cancers or cancer. Biopsy procedure is discussed later in the article briefly. If you are interested to read more about biopsy, please check this DiseaseFix article that is available separately – Biopsies for Cervical Cancer.
The doctor may put a weak solution of acetic acid on your cervix to make any abnormal areas easier to see. If an abnormality is seen, a biopsy (involves removal of a small piece of the tissue from the target site) will be done. A biopsy is the best way to tell with certainty whether an abnormal area is a pre-cancer, a cancer, or neither of them.
Although the procedure is usually not very painful, the cervical biopsy can cause discomfort, cramping, bleeding, or even pain in some women. Colposcopy requires no anesthesia and the level of discomfort is usually similar to that of the discomfort caused by a Pap smear in most women.
Biopsy
It involves removal of a small amount of tissue for examination under a microscope. Other tests can suggest that cancer is present, but only a biopsy can make a definite diagnosis of the cervical cancer.
The cells are extracted and then analyzed by a pathologist in a lab setting. A pathologist is a doctor who is specialized in analyzing and interpreting the laboratory tests to diagnose a disease. If the lesion or tumor or cancerous tissue is small, the doctor may remove all of it during the biopsy only.
There are several types of biopsies, such as:
- An instrument is used to pinch off small pieces of cervical tissue
- Endocervical curettage (ECC): If the doctor wants to check an area inside the opening of the cervix that cannot be seen during a colposcopy, she may do a procedure called endocervical curettage (ECC). A small instrument called a curette is used to scrape a small amount of tissue from inside the cervical opening.
- Loop electrosurgical excision procedure (LEEP): This procedure uses an electrical current to be passed through a thin wire hook. The hook removes tissue for examination.
- Conization (a cone biopsy): It removes a cone-shaped piece of tissue from the cervix. It is done to remove a pre-cancer or an early-stage cancer. Conization is done under a general or local anesthetic in the hospital.
If the biopsy shows the evidences of cervical cancer, the doctor may order additional tests to see if the cancer has spread beyond the cervix and to determine the stage of the cervical cancer.
X-ray
An x-ray is used to create pictures of the structures inside of the body with the help of radiation-based procedures.
Computed tomography (CT or CAT) scan
A CT scan creates a 3-dimensional image of the inside of the body using x-rays. A computer is connected to the CT scan machine to create detailed, cross-sectional views that show any abnormalities or cancers.
A CT scan can help measure the size of a tumor. Generally, a special dye called a contrast is injected before the scan for better views on the image. This dye can be injected into a patient’s vein or given as a pill to swallow.
Magnetic resonance imaging (MRI)
An MRI uses powerful magnetic fields (and not x-rays like in CT scan) to produce detailed images of the body.
MRI can help measure the size of a tumor. A special dye called a contrast is given before the MRI scan also to create a better images. This dye can be injected into a patient’s vein or given as a pill to swallow.
Proctoscopy (also called a sigmoidoscopy)
A proctoscopy is a test that allows the doctor to see the entire colon and rectum with a thin, lighted, flexible tube called a sigmoidoscope.
The person may be sedated as the tube is inserted in the rectum. It help see if the cancer has spread to the rectum.
Positron emission tomography (PET) or PET-CT scan
A PET scan is usually combined with a CT scan and is called a PET-CT scan. A PET scan is used to create pictures of organs and tissues inside of the body.
A small amount of a radioactive agent is injected into the body. This substance is consumed by the cells that use the most energy. Since cancer tends to use most energy, it absorbs more of the radioactive substance. A scanner can detect this pattern of energy usage by the cells to produce images of the inside of the body and indicate which regions have cancerous cells.
Cystoscopy
A cystoscopy is a diagnostic method to help view the inside of the bladder and urethra with a thin, lighted tube called a cystoscope. The person may be given drugs for sedation as the tube is inserted in the urethra.
A cystoscopy is used to determine whether the cancer has spread to the bladder.
Treatment of cervical cancer
Treatment of cervical cancer varies for each patient. Cervical cancer treatment depends on the stage of the disease. The stage of a cervical cancer describes its size, depth of invasion and how far the cancer has grown into the cervix, and how far it has spread to other locations.
After establishing the stage of your cervical cancer, treatment options will be identified for your condition. Your cancer team will suggest what they think might be the best treatment options, but the final decision will be yours.
Common types of cervical cancer treatments include:
- Surgery
- Radiation therapy
- Chemotherapy (also referred to as chemo simply)
- Targeted therapy
Surgery for treating cervical cancer
There are three main types of surgical methods for cervical cancer treatment. They are:
- Radical trachelectomy – in this procedure, the cervix and surrounding tissue and a part of the vagina are removed. The womb (uterus) is not removed.
- Hysterectomy – the cervix and womb are both removed in this surgery depending on the stage of the cancer. Sometimes, the ovaries and fallopian tubes may also be removed.
- Pelvic exenteration – it involves major surgery in which the cervix, vagina, uterus, bladder, ovaries, fallopian tubes and rectum are all removed.
Radiotherapy
Radiotherapy may be used to treat cervical cancer on its own. Sometimes, it may be combined with surgery for early stage cervical cancer or with chemotherapy for advanced cervical cancer.
It can be delivered in these ways:
- externally – a beam of high-energy waves are delivered into the pelvis to destroy cancerous cells
- internally – a radioactive implant is placed inside the vagina and cervix
- in some cases, a combination of internal and external radiotherapy is used
Radiotherapy can sometimes harm healthy tissue as well in addition to damaging the cancer cells. However, the benefits of radiotherapy often outweigh the risks. Sometimes, it is the only hope of getting a cure for the cancer.
Chemotherapy
Chemotherapy can be delivered with radiotherapy, or as a standalone treatment in itself for advanced cancer to slow its progression.
Chemotherapy can include either a single medication or a combination of different chemotherapy medications to kill the cancerous cells. Chemotherapy is usually given using an intravenous mode on an outpatient basis.
Targeted therapy
Targeted therapy is the use of drugs that have been specifically developed, or targeted, to interrupt cellular processes that promote growth of the cancer cells. Bevacizumab (Avastin) is one such drug used in targeted therapy. It inhibits the ability of tumors to make new blood vessels, which is required for tumor growth.











