Achalasia: Causes, Symptoms, Diagnosis, Treatment
- Updated on: Jul 10, 2024
- 5 min Read
- Published on Jan 31, 2019
Understanding Achalasia: Definition and Overview
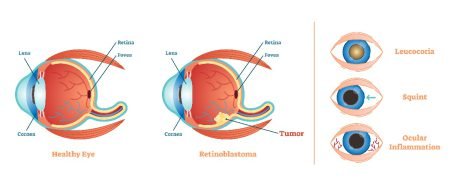
Achalasia is a rare disorder of the esophagus. It becomes difficult to swallow any type of solid or fluid food if a person has achalasia. It is observed that the nerves in the esophagus become damaged and the muscular valve between the esophagus and lower esophageal sphincter (LES) or the stomach is not relaxed. The valve stays closed even during swallowing which becomes it difficult to squeeze down the food. The term ‘Achalasia’ is derived from a Greek term “chalasis” which means slackening.
The function of the esophagus is to transport food from the mouth to the digestive system. The esophagus is a hollow tube divided into: the uppermost part or the upper esophageal sphincter, the body of the esophagus, and the lower esophageal sphincter. The upper part distinguishes the esophageal tube from the throat, the body or the tube carries the food downwards and the lower sphincter transfers the food to the stomach and remains closed (as a valve) to avoid the food and acids from backing up from the stomach.
Achalasia is referred to as esophageal peristalsis also. It occurs in only 1-2 people in 200,000 and is most common in adults of ages 30 to 60. It was estimated that about 10 to 12% of all patients with achalasia are children or teenagers. Cleveland Clinic says that achalasia affects about 3,000 people in the United States every year. Another name of achalasia is cardiospasm.
Causes of Achalasia
The actual cause of achalasia is not known but some scientists believe that it may occur due to an autoimmune condition. Some also predict that the damage to the nerves of the esophagus might occur due to a viral infection, or due to conditions such as Chagas disease, degeneration of Auerbach’s plexus, etc. Some fear that it might be inherited, but there is no evidence for it as yet.
Symptoms of Achalasia in Esophagus
Most common signs and symptoms of Achalasia are:
- The most common symptoms of achalasia is dysphagia of the esophageal mucosa. Dysphagia slowly progresses over the years and leads to difficulty in swallowing both, solid and liquid foods. Dysphagia results in chest pain or retrosternal pain and expulsion of food (that has not entered the stomach). This can often also lead to a risk of aspiration or choking.
- Weight loss occurs in a few months due to not having the food.
- In some cases, severe infections such as bronchopulmonary infections or pneumonia (7% to 8% patients) are also observed.
- Heartburn, intense pain or discomfort is felt after eating.
- Some other symptoms, which are non-specific to the disorder, are also observed such as hiccups, difficulty in burping, foul-smelling burps, excess formation of saliva etc.
If these signs are ignored in the beginning, the chances of getting esophageal cancer are heightened.
Diagnosis of Achalasia
Early achalasia diagnosis is recommended for proper treatment. Esophageal achalasia can easily be diagnosed during a chest X-ray but some specific tests are recommended to confirm the diagnosis.
Barium swallow test
Barium swallow is one the most common tests for diagnosing achalasia. A white liquid containing the chemical, barium, is taken in and then an X-ray scan is done. Barium in the liquid coats the inside of the esophagus and the stomach to provide a clear picture during the X-ray. During this test, the absence of progressive peristaltic contractions while swallowing is observed. Also, the lower part of the esophagus is observed to be narrowed whereas the upper part seems to be stretched.
Another test known as ‘Gastrografin swallow’ may be recommended by your doctor. This test works in the same way as Barium swallow works except that gastrografin is used in this case, which causes lesser irritation in case of a leak from the oesophagus.
Esophageal manometry
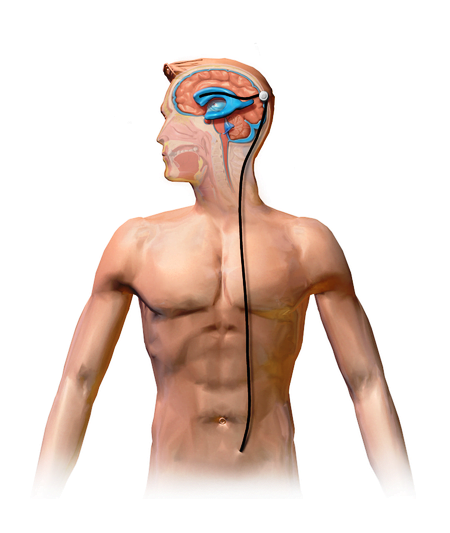
Manometers are used to measure fluid pressure. During esophageal manometry, a tube is placed in the esophagus to record muscle contractures (timing and strength of the muscle) while swallowing and to monitor coordination and force exerted by esophagus muscles. The device also helps to regulate relaxation of the lower esophageal sphincter while swallowing.
For esophageal manometry, a thin tube is made to propel through the nose, down the throat into the esophagus to measure the pressure within the LES and also measure the aperistalsis in esophageal body.
Gastroscopy or Endoscopy
During endoscopy, a thin, flexible fiberoptic tube with a light and camera (endoscope) is passed through the throat to examine the inside of the esophagus and stomach. Endoscopy is helpful in determining a partial blockage of the esophagus if a possibility is suspected.
Endoscopy can also be used to collect a sample of tissue (biopsy) to test for complications of reflux such as Barrett’s esophagus, etc. During gastroscopy, a sample of tissue from the esophagus or stomach might also be taken for biopsy. This is done to rule out or to diagnose any other severe abnormalities such as esophageal cancer and to find other causes of dysphagia.
Achalasia Treatment
The treatment of achalasia results in improving the symptoms of achalasia. No treatment however is available that can repair the damaged nerves or restore normal contractions in the esophagus. Achalasia can be treated by both, non-surgical and surgical methods.
Non surgical treatment for Achalasia
- Balloon dilation: More than 65% of the patients of achalasia are treated through balloon dilation method. It involves the dilation or stretching of the sphincter at the base of the esophagus by placing a small balloon inside the sphincter and inflating it. This method is also known as pneumatic dilation. This process needs to be repeated within every 5-6 years of the prior procedure. The risk of esophagus to rupture is also high during the procedure.
- Botox (botulinum toxin type A): Injections of muscle-relaxing medicine- Botox (botulinum toxin) are given into the sphincter through an endoscope. These injections are recommended to patients who cannot undergo pneumatic dilation or surgery either due to age or overall health. Botox injections are recommended as temporary treatment to relax muscles.
- Usage of Drugs: Drugs such as nitrates or calcium channel blockers (isosorbide dinitrate (Isordil), nifedipine (Procardia), etc) are used to relax the lower esophageal sphincter. Some of these medicines might also have severe side effects.
Surgical Treatment of Achalasia
In case of severe achalasia, a minimally invasive surgical technique called Laparoscopic esophagomyotomy or Heller Myotomy is recommended. More than 90 percent of people are found to get relief from symptoms of achalasia after the surgery. A small cut is made in the lower esophageal sphincter muscle to release the tension and relax the muscles. Sometimes, this method results in complications such as tearing of the esophagus, development of gastroesophageal reflux disease (GERD), etc. To prevent GERD, esophagomyotomy can be combined with anti-reflux surgery (fundoplication). The top portion of stomach is wrapped around the lower esophageal sphincter to tighten the muscle and prevent acid reflux.
Another surgical method which is used as a treatment for achalasia is called peroral endoscopic myotomy, or POEM. In this method, no external cut is made in the body but an endoscope is inserted into the throat and a small cut is made in the internal lining of the esophagus to make swallowing easier.
After surgery, some patients may suffer from bad heartburn symptoms. It is also seen that in some cases, both, non-surgical and surgical treatment are needed.