Castleman’s Disease: Emerging Treatments
- Updated on: Jul 10, 2024
- 3 min Read
- Published on Sep 20, 2019
Latest research on Castleman’s disease
Study of several new drugs against Castleman’s disease in recent years can be promising. Multiple studies on interleukin-6 proteins, monoclonal antibodies, corticosteroids, etc have gained significance in recent years for the treatment of this disease. Several clinical trials are being conducted on cancer cells and on animals to understand the outcome of the treatment for Castleman’s disease.
Before any drug is considered for human testing, it first needs an approval by the US Food and Drug Administration (FDA) as an assurance that the drug to be investigated is safe for human clinical trials. In many cases, new treatments may yield different results which can be conflicting. Conflicting results occur due to study design problems or other factors which affect the outcome of the treatment on the patient. Here are some new evidences from research associated with Castleman’s disease.
Medidata collaboration sheds light on rare diseases: Need and value of precision medicine
Medidata initiates to discover new drug targets or biomarkers for Castleman’s disease. By collaborating with CDCN (Castleman Disease Collaborative Network), Medidata has discovered six new patient subsets reflecting either distinct subtypes or proteomic disease states for iMCD and also, has provided evidences of proteomic predictors of anti-interleukin-6 treatment response.
This Medidata trial fulfills goals of personalized medicines as it aims to discover new drugs which are more effective for the disease subtypes i.e. to understand the etiological insights of poorly understood rare diseases and new potential drug targets.
A doctor’s research trek into his own rare disease
Dr. David Fajgenbaum was diagnosed with a rare immune system disorder, in 2010, when he was in his third year of pursuing medicine. He realized a sudden fall in his health condition and was then diagnosed with idiopathic multicentric Castleman disease (iMCD). It is known that this rare condition kills about 35 percent of its victims within five years of diagnosis.
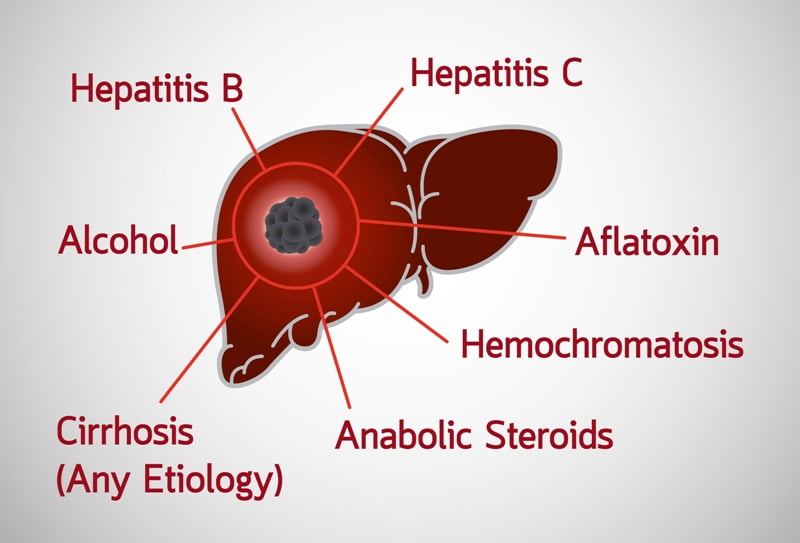
Castleman disease, also sometimes referred to as giant lymph node hyperplasia or angiofollicular lymph node hyperplasia, affects lymph nodes in any part of the body. In this condition, a large quantity of inflammatory proteins are released which hinder the normal functioning of the liver, kidneys and bone marrow. Castleman’s disease can be classified into unicentric CD (UCD), HHV-8-positive multicentric CD (MCD) and HHV-8-negative MCD (also called idiopathic MCD or iMCD).
After recovering from the condition, Dr. Fajgenbaum started making efforts to find a proper treatment for Castleman’s disease. Currently, he is heading a clinical trial on Sirolimus, an immunosuppressant which is used during kidney transplants to avoid rejections. Sirolimus can be beneficial during the treatment of autoimmune diseases and therefore is being studied for Castleman’s disease also.
These clinical trials on sirolimus were initiated after 344 studies helped to standardize the first three lines of treatment for iMCD by introducing siltuximab as the best drug with 85 percent success rate.
Emerging use of biologics for Castleman’s disease
Anti-IL-6 therapy and use of monoclonal antibodies such as Siltuximab, Tocilizumab, etc are rising and promising measures to improve the patient’s response rates and are recommended as more durable disease control methods.
A research study entitled “Castleman’s Disease: From Basic Mechanisms to Molecular Therapeutics” stated that the contribution of IL-6 to the pathogenesis of Castleman’s disease was studied on animal models. By using an anti–IL-6 receptor (IL-6R) monoclonal antibody, the effect of blocking IL-6 in transgenic mice carrying human IL-6 cDNA was studied. During the study, the ‘control mice’ was observed to develop anemia, plasmocytosis, thrombocytosis, mesangial proliferative glomerulonephritis, leukocytosis, etc. After this, it was concluded that the mice who received the monoclonal antibody did not develop these symptoms and lived longer than the other.
These emerging biologics have great potential in treating HIV- and HHV-8-negative cases. As research is still under trials, the underlying disease mechanisms for Castleman’s is still not understood.