COPD Exacerbations
- Updated on: Aug 17, 2024
- 4 min Read
- Published on Oct 17, 2019
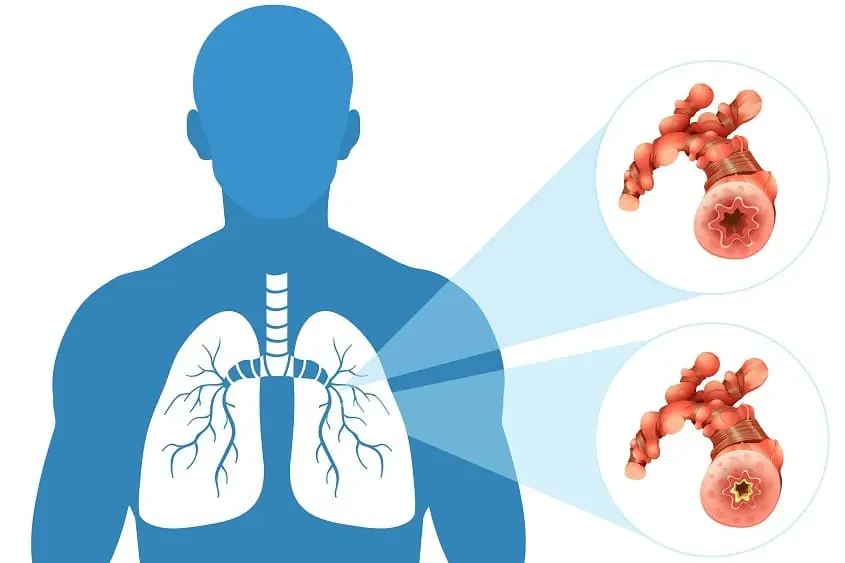
COPD or chronic obstructive pulmonary disease is a group of diseases that cause airflow blockage and extreme breathing problems in people to the point of breathlessness. Most commonly, COPD includes emphysema and chronic bronchitis. Besides, COPD also includes bronchiectasis and, in some patients, asthma too. With its progression, COPD gets worse and, in later stages, people may experience extreme breathlessness at all times, even when they are sitting still.
About COPD Exacerbation
Chronic obstructive pulmonary disease often goes undiagnosed and can be fatal if not treated properly. An acute COPD exacerbation refers to a flare-up or episode where a person’s breathing becomes worse than normal and can lead to life-threatening complications depending on the cause and severity of disease.
COPD exacerbations are major setbacks for people with the disease. By understanding the risk factors and identifying the symptoms, a person can get proper treatment before the situation becomes life-threatening. In later stages of the COPD, people may need to go to the hospital, but if there are less severe exacerbations, they may be able to manage them at home. People with COPD should work with their doctors and medical team to make sure that everyone understands what should be done when exacerbations occur. The best way to prevent or lower the risk of exacerbations is to understand the risk factors, know the signs and symptoms, and have an action plan in place.
Signs of COPD Exacerbations
COPD exacerbations are sudden flare ups in acute respiratory symptoms in people diagnosed with severe COPD. These exacerbations are concerning because they cause difficulties in an already serious condition. With COPD, any damage incurred by the lungs tends to be permanent and therefore may end up pacing the progression of the disease. By understanding triggers of COPD exacerbations, people may be able to avoid flare-ups or better manage the symptoms if and when they begin.
When people have severe COPD, their usual symptoms become worse quickly and this is called as an exacerbation or a flare-up. During one of these bouts, people may suddenly have more trouble in breathing or make more noise when they breathe. These flare-ups are frequently linked to a lung infection caused by a virus or bacteria, like cold or some other illness. Smoggy or dirty air can also make the symptoms worse. It’s important to know the warning signs of exacerbations or flare-ups so that they can be avoided if possible. Exacerbations can make COPD worse and the person can be hospitalized. Some early warning signs of a flare-up include:
Shortness of Breath
It is one of the obvious signs of an oncoming flare-up. If you are feeling breathless, it can be a warning sign of an exacerbation. In COPD patients, it usually happens during light physical activities or even at rest.
Noisy Breathing
Noisy breathing or wheezing means that mucus or pus is blocking airways and can be a warning sign for exacerbations.
Worse Coughing
One of the important signs of an exacerbation or a flare up is a severe cough which can be dry or brings up green, yellow or bloody phlegm.
Changes in Skin or Nail Color
A bluish tint around lips, blue or purple color nails, and yellow or grey skin can be a warning for upcoming exacerbations.
Some other warning signs of COPD exacerbations are:
- Trouble sleeping and eating
- Inability to talk, a late and dangerous sign of worsening breathing
- Early-morning headaches because of a buildup of carbon dioxide in blood
- Swollen ankles or legs and belly pain
- High fever, an important sign of infection and an oncoming flare-up
Self awareness is important when it comes to COPD flare-ups. Only a person himself can know how he feels on a typical day, how his breathing feels and how much he coughs. Paying close attention to all these things can be helpful.
Causes
A COPD exacerbation is usually triggered by inflammation in the lungs, caused by an infection or irritants. Few examples include:
- Pneumonia
- Flu
- Seasonal allergens
- Air pollution
- Smoke
People with COPD should take all possible steps to avoid lung infections, such as getting flu shots annually. They may also need pneumococcal vaccines because lung infections can also lead to exacerbations.
Almost 33 % of COPD exacerbations have an unknown cause. Bacterial and viral infections of the lungs ( like pneumonia) are common triggers for COPD in the same way as smoking, air pollution, exposure to toxic fumes, strong odors, and airborne allergens such as dust, pollen, and pet dander.
COPD exacerbations are more commonly found in individuals who are either being undertreated or are not following the prescribed therapy. Among persons provided treatment, exacerbations are more expected to occur if:
- Smoking is not stopped completely
- Short and long-term inhalers are improperly used
- Oral medications are not taken as prescribed
- The person relies completely on drug treatment and doesn’t participate in pulmonary rehabilitation programs.
Because COPD differs among different individuals, one should work with doctors to design a treatment plan appropriate for his/her condition and lifestyle. There is no one-size-fits-all solution in case of COPD.
COPD Exacerbation Treatment
COPD exacerbations are often treated with rescue bronchodilators that help in opening the airway passages and reduce inflammation. Other treatments can also be used depending on the stage of COPD and the severity of its symptoms. These include:
- Oxygen therapy
- Glucocorticosteroids (usually inhaled during flare-ups)
- Respiratory stimulants
- Antibiotics for treating any underlying bacterial infection
Top Prevention Tips for Exacerbations
Prevention is always the best approach to managing COPD exacerbations. In addition to taking prescribed medications, the incidence of flare-ups can be reduced in the following ways:
- Avoiding smoking by engaging in a fully supported treatment program.
- Getting immunized with pneumococcal vaccines and booster shots.
- Getting annual flu shots to reduce the risk of some serious illnesses
- Exercising regularly to improve cardiovascular and respiratory capacity.
- Eating a balanced diet to either lose weight if you are obese or gain weight if you are underweight.
- Washing hands regularly to avoid infections.
- Avoiding crowds during cold and flu seasons.
- Seeing an allergist if you are prone to seasonal allergies.
- Avoiding clogging of inhalers and keeping extra stock, so that you never run out of inhalers when required.
Sleeping properly so as to keep your immune system in the best shape possible.