Cellulitis in Adults – Overview
- Updated on: Jul 16, 2022
- 4 min Read
- Published on Jul 15, 2022
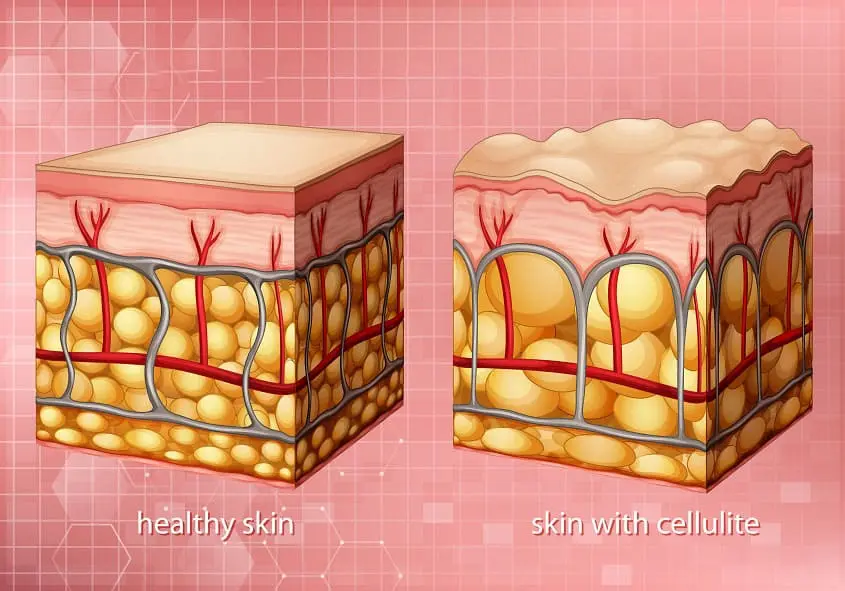
Skin infections called cellulitis are most frequently brought on by the bacteria Streptococcus or Staphylococcus. These bacteria can penetrate the skin through microscopic fissures, which is how redness, swelling, and warmth in the skin suddenly occur. The symptoms of cellulitis might occasionally include fever, chills, and general exhaustion.Cellulitis may lead to abscesses or the spread of bacteria into the circulation if the infection is not treated in a timely manner (bacteremia). The majority of cellulitis infections do, however, get well with the right antibiotic medication.
Why Does Cellulitis Occur?
Bacteria typically penetrate a wound or an area where there is no skin to develop cellulitis. Cellulitis is most frequently brought on by the following bacteria:
- Hemolytic streptococcus, group A ß (Strep)
- pneumococcal streptococcus (Strep)
- Staphylococcus (Staph)
In healthy individuals, staph and strep bacteria are frequently found on the skin, as well as the mucous membranes of the mouth and nose. When the skin is broken and the bacteria are able to enter, an infection results. Bites from people or animals or injuries sustained while swimming are examples of additional reasons.
Symptoms and Signs
Any area of the body can develop cellulitis, although the following are the most typical sites:
- Reduced legs
- hands or arms
- Face
Pink to red, mildly irritated skin is how cellulitis initially manifests itself. As the infection grows, the affected area may quickly develop deeper redness, swelling, warmth, and tenderness. On rare occasions, crimson streaks may extend from the cellulitis. There may also be lumps with pus inside them or blisters.Fatigue, fever, chills, and enlarged lymph nodes can all be symptoms of cellulitis.
Symptoms may vary from person to person. Typical signs include:
- Skin that is flaming red
- Inflammation of the skin
- Tenderness
- A warm body
- Pain\Bruising
- Blisters
- Fever
- Headache
- Chills
- Weakness
- Red streaks from the cellulitis’s original place
Cellulitis can occasionally result in an emergency. Always get in touch with your doctor right away if you have any of the following symptoms:
- A sizable patch of skin that is red and irritated
- Fever
- If the affected area is creating alterations in a hand, arm, leg, or foot, such as numbness or tingling
- If the skin seems dark
- If the area surrounding your eye(s) or behind your ear is red and swollen
- If you acquire cellulitis and have diabetes or a compromised immune system
Cellulitis symptoms can resemble those of other skin disorders. For a diagnosis, always consult your healthcare provider.
When to Get Medical Attention
Make an appointment with your doctor as soon as you see a sore, swollen, heated, or red spot on your skin. Cellulitis should be treated as once to prevent complications from developing. You should visit the emergency department if you have a fever, chills, or the injury is to your face.Visit your doctor again if your skin infection is presently being treated and doesn’t get better after 2-3 days of antibiotics. The infection may have spread deeper into your skin, or you may need to be treated with other treatments.
Methicillin resistance in the community A kind of “staph” bacteria called Staphylococcus aureus (CA-MRSA) is resistant to drugs of the penicillin family. For many years, this class of antibiotics has served as the mainstay of treatment for staph and skin infections. Only a small portion of the population, such as healthcare personnel and drug injectors, has previously been exposed to CA-MRSA. But in the general community, CA-MRSA is now a frequent source of skin infections. Despite the fact that CA-MRSA bacteria are resistant to penicillin and medications that are linked to penicillin, the majority of CA-MRSA infections are easily treatable using widely accessible nonpenicillin antibiotics. Rarely, CA-MRSA might result in a deeper skin infection that needs to be treated with intravenous (IV) antibiotics.Hospitalization is frequently required for effective treatment since there is another strain of MRSA (hospital-acquired MRSA), which is typically prevalent in health care settings. This strain is only responsive to intravenous antibiotics.
Treatments Your Doctor May Recommend
Cellulitis is typically quickly identified by your doctor after inspecting the affected area. In order to identify the precise bacterium causing the cellulitis and test its susceptibility to various antibiotics in order to help inform treatment choices, your doctor may occasionally request blood tests and/or conduct a bacterial culture.
If there are lots of bacteria present, the lab will typically have early findings in 48–72 hours. The complete results of the culture, however, might not be seen for a whole week or longer. The laboratory typically conducts antibiotic sensitivity testing in order to find the antibiotics that will be most effective in treating the bacteria, as addition to determining the type of bacterium that is causing the cellulitis.
Your doctor might prescribe an antibiotic to treat the most typical bacteria that cause cellulitis while you wait for the results of the bacterial culture. Your doctor might switch the antibiotic you’re taking after the final culture results are in, especially if the illness isn’t getting better.
Oral antibiotic tablets can be used to treat mild cellulitis in healthy individuals. The following are typical antibiotics that are used to treat cellulitis:
- Dicloxacillin
- Cephalexin
- Trimethoprim-sulfamethoxazole
- Clindamycin
- Doxycycline
- Linezolid
It may be necessary to hospitalize someone in order to receive intravenous antibiotics if they look to be severely ill or if they have other chronic illnesses that could make recovery more difficult. The following intravenous antibiotics are frequently used to treat cellulitis:
- Nafcillin
- Oxacillin
- Cefazolin
- Vancomycin
Make careful to finish the entire course of antibiotics if your doctor recommends them. Your doctor will probably want to make sure that your underlying medical issues, if any, are being properly handled in addition to giving antibiotics.