Infective Endocarditis and Drug Abuse
- Updated on: Jul 11, 2024
- 5 min Read
- Published on Nov 25, 2019

Endocarditis in Intravenous Drug Abusers
Infective endocarditis (IE) is one of the most severe complications in patients who are intravenous drug abusers (IVDA). It usually affects the heart’s tricuspid valve and staphylococcus aureus infection is the most common etiologic agent with a relatively good prognosis.
Current reports suggest that almost 40% to 90% of intravenous drug abusers (IVDA) with infective endocarditis are HIV infected, and the HIV epidemic has decreased the prevalence of this disease, perhaps due to changes in drug-abusing habits by addicts for avoiding HIV transmission.
Drug abuse is one of the major factors for infective endocarditis and patients who suffer from drug abuse infective endocarditis (DA-IE) have significant morbidity and mortality. Centers for Disease Control and Prevention suggest that the admissions for infective endocarditis in patients aged below 30 years with IVDA increased from 11% in 2008 to 27% in 2014. Also, it was found that there was a double-fold increase in infective endocarditis-related deaths among young people aged below 35 years.
In the national opioid epidemic, there has been an increase in the incidence of drug abuse (DA). With this increase in DA, the risk for infective endocarditis has also increased. However, there is limited current data that can evaluate national trends on the incidence and geographical distribution of drug abuse infective endocarditis (DA?IE).
Drug abuse (DA) continues to increase in the United States. In 2016, the number of deaths due to an opioid?related drug overdose has increased 5 times than in 1999. Heroin drug?related deaths nearly tripled during this period. In the year 2017, the United States “Department of Health and Human Services” declared the US opioid epidemic a public health emergency. This opioid epidemic has increased infectious?related morbidity and mortality including infective endocarditis.
Effects of Infective Endocarditis in Intravenous Drug Abusers (IVDA)
Based on location, infective endocarditis in active intravenous (IV) drug users can be divided in different scenarios:
- Right-sided endocarditis is one of the most common presentations (70% of all cases) of infective endocarditis in IV drug users which usually involves the tricuspid valve, and a murmur may not be always present. Symptoms are generally non-specific and may include fever, pleuritic chest pain, dyspnea, and non-productive cough. Right-sided endocarditis has a good prognosis, with a survival rate above 95%.
- Left-sided endocarditis is very relevant to disease in non-IV drug users, but it can be linked to systemic manifestations from embolic events. It should be noted that renal, splenic and central nervous system involvement requires a special attention, as they can mask the initial presentation of the disease.
- Intrinsic pulmonary hypertension due to lung parenchymal damage is one of the risk factors for right-sided endocarditis. Right-sided endocarditis is most often seen with a normal valve (based on autopsy series).
Risk Factors of Infective Endocarditis in Drug Abusers
Risk factors of infective endocarditis in drug abusers mainly include:
- Concomitant infection at other sites
- Colonization of staphylococcus aureus
- Inexperienced user
- HIV infection with CD4 count less than 200 cells/cubic millimeter
- Injecting cocaine
- Any previous history of infective endocarditis
- Male gender (ratio varies from male to female ratio about 2:1 to 5:1)
Complications of Infective Endocarditis in Drug Abusers
Some of the main complications of infective endocarditis in IVDA include:
- Septic pulmonary emboli with right-sided endocarditis
- Pneumothorax associated with septic pulmonary emboli
- Congestive heart failure
- Valvular insufficiency
- Pneumonic consolidations and pleural effusions
- Myocarditis
- Pericarditis
- Myocardial infarction due to coronary emboli
- Stroke
- Meningitis
- Brain abscess
- Endophthalmitis
- Immune-complex mediated glomerulonephritis
- Osteomyelitis and septic arthritis
- Myocardial abscess
These are some key points to remember about infective endocarditis in IV drug users:
- Right-sided endocarditis has a good prognosis with a survival rate greater than 90%
- Left-sided endocarditis has a bad prognosis.
- Vegetations greater than 2 cm are often associated with worse outcomes
- Infections due to fungi often have a higher mortality
Correlation Between Heart Infections and Opioid Addiction
On September 18, “The American Heart Association” published a study in its official journal which reports that the opioid epidemic has led to an increase in heart infections throughout the United States. The researchers reached the conclusion by analyzing the National Inpatient Sample Registry, a database of hospitalizations across the country. The number of American drug abusers who went to the hospital for infective endocarditis doubled from 8% to 16% from 2002 to 2016. To address this dreadful problem, Dr. Harb says that treatment for opioid addiction is essential for preventing more cases of drug-related infective endocarditis.
It is very unfortunate that, patients who survive opioid-induced heart infections can never receive treatment for their substance use disorders. Therefore, they may develop infections again. Also, these patients are found to be more susceptible to infective endocarditis for the second time compared to patients who are non-drug users. Therefore, the researchers recommend that the treatment for infective endocarditis in IV drug users should also involve treatment for their addiction, specifically for demographics that are most at risk.
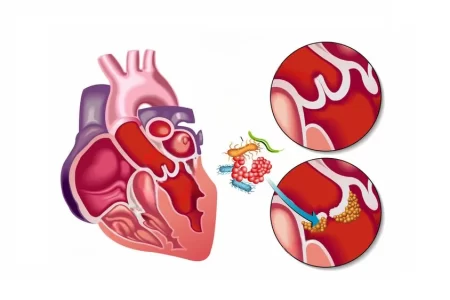
Right-Sided Infective Endocarditis (RSIE) and Intravenous Drug Abuse
Right-sided infective endocarditis is mainly caused due to IV drug abuse. Although, right-sided infective endocarditis is rare, it comprises 5–10% of all infective endocarditis cases. Right-sided infective endocarditis is more common in patients with medical devices such as pacemakers and defibrillators and dialysis catheters.
Recently, there is found an increase in right-sided infective endocarditis cases due to intravenous drug abuse. Right-sided infective endocarditis due to IV drug abuse most commonly affects the tricuspid valve and rarely the pulmonary valve. Even though the majority of uncomplicated cases of right-sided infective endocarditis due to IV drug abuse do well with medical treatment, it is linked with substantial morbidity and mortality due to recurrent infection. Surgical options for right-sided infective endocarditis are very uncommon particularly, in resource-limited setting. However, some current studies have investigated surgical options in such patients.
Intravenous drug abuse (IVDA) is a known risk factor for infective endocarditis. Intravenous drug users are at a seven times higher risk for infective endocarditis compared to patients with other diseases like rheumatic heart disease. Over the last decade, there has been a rapid increase in the number of cases related to infective endocarditis due to intravenous drug use. Between 2000 and 2008 the rate of IV drug abuse-related infective endocarditis has increased from 6 to 8% hospitalization to 12% in the year 2013 (Reference: Increasing infectious endocarditis admissions among young people who inject drugs; Open Forum Infectious Diseases,2016).
According to a study published in “Trends in drug use-associated infective endocarditis and heart valve surgery, 2007 to 2017: A study of Statewide discharge data, Annals of Internal Medicine”, it is reported that there has been a 12-fold increase in hospitalizations for intravenous drug use-related infective endocarditis over the last decade in the United States and North Carolina.
In IVDA patients, the right side infective endocarditis (RSIE) accounts for 5–10% of cases. RSIE may also occur in patients with intra cardiac devices like pacemakers and defibrillators but it is often associated with HIV infection in IV drug users.
How is Infective Endocarditis Diagnosed in IVDA Patients?
Initial symptoms are mostly non-specific and mainly include fever (not in all cases), weight loss, fatigue, pain in chest, shortness of breath (which may be due to both heart failure from valvular dysfunction and septic emboli), or genitourinary symptoms like hematuria, flank pain, and glomerulonephritis.
History of patients may include:
- Recent use of intravenous drugs
- Damage of nasal mucosa from drug use
- Earlier history of infective endocarditis and intravenous drug use
Cardiac examination of IVDA-IE patients may include a new murmur or a change in the characteristic of a murmur present before the disease. Chest radiographs can show complications related to infective endocarditis like heart failure signs, pulmonary findings that can suggest embolization or concomitant infection, and soft tissue infections. Some dermatological findings like Roth’s spots, Osler nodes, and Janeway lesions, are rarely found in this group of patients.
How to Prevent Infective Endocarditis in IVDA Patients
One of the best ways to prevent infective endocarditis in IVDA patients is stopping intravenous drug use so that we can prevent associated infections, but this is not always possible. However, treating endocarditis in IV drug users provides an opportunity to intervene in this self-destructive behavior. Strenuous efforts can be made to refer these patients into programs that provide medication-assisted treatments (methadone, buprenorphine-naloxone) and are an imperative part of treating IV drug-related endocarditis.
Endocarditis prophylaxis can be recommended to patients with an early history of endocarditis, who have overcome addiction as well as stopped IV drug use (recommended by the American Heart Association).
In some cases where treatment-related to addiction has been rejected, some risk-reducing strategies (like syringe-exchange programs, educational interventions for improvement of techniques and use of paraphernalia, and providing naloxone for overdose treatment) can help in reducing future infections and death due to drug overdose.