Basic Overview of Thalassemia
- Updated on: Jul 6, 2024
- 5 min Read
- Published on Jul 22, 2021
What is Thalassemia?
Thalassemia is a hereditary blood disorder characterized by less hemoglobin and a smaller number of red blood cells in the body than normal. Hemoglobin is a substance in our red blood cells that helps in the transport of oxygen in our body. Due to the presence of less hemoglobin and small red blood cells, thalassemia results in anemia leaving a person fatigued.
Thalassemia is inherited, which means that at least one of the parents should be a carrier of the disease. Thalassemia can be mild or severe. Mild thalassemia does not need any treatment while a severe form of the disorder requires regular blood transfusions. In thalassemia, the body makes an irregular form or insufficient amount of hemoglobin. In this disorder, a large number of red blood cells get destroyed, which ultimately leads to anemia. Anemia is a condition in which the body lacks enough normal, healthy red blood cells. Severe anemia caused due to thalassemia can result in organ damage.
Thalassemia is usually caused by either a genetic mutation or by removal of certain key gene fragments. There are two main forms of thalassemia that are more severe. One is alpha thalassemia and the other is beta thalassemia. In alpha thalassemia, at least one of the alpha globin genes is mutated or has some kind of abnormality while in beta thalassemia, the abnormality is found in beta globin genes.
What are the different types of thalassemia?
Thalassemia has three main types and four subtypes and all of types and subtypes vary in symptoms and severity. The types and subtypes of thalassemia are:
- Beta thalassemia with subtypes major and intermedia
- Alpha thalassemia, with subtypes hemoglobin H and hydrops fetalis
- Thalassemia minor
Beta Thalassemia
Beta thalassemia occurs when the body is unable to produce beta globin. This type of thalassemia has two subtypes: thalassemia major or Cooley’s anemia and thalassemia intermedia.
Thalassemia Major
It is the most severe form of beta thalassemia and develops when beta globin genes are absent. The symptoms of thalassemia major usually appear prior to a child’s second birthday. This condition results in a severe anemia which can be life-threatening. Signs and symptoms of thalassemia major are fussiness, jaundice, lack of appetite, frequent infections, yellowing of the skin, enlarged organs etc. Thalassemia major is a serious form of thalassemia and it often requires regular blood transfusions.
Thalassemia intermedia is a less severe form. It occurs due to alteration in both beta globin genes. People with thalassemia intermedia don’t need blood transfusions.
Alpha Thalassemia
Alpha thalassemia occurs when the body is unable to produce alpha globin. It has two subtypes- hemoglobin H disease and hydrops fetalis.
Hemoglobin H
This is a subtype of alpha thalassemia in which a person either lacks three alpha globin genes or undergoes some changes in these genes. This disease results in certain bone diseases and also causes the overgrowth of cheeks, forehead, and jaws. The disease may cause jaundice, enlarged spleen and malnourishment.
Hydrops fetalis
This subtype of alpha thalassemia is an extremely severe form of thalassemia that occurs in fetus. Most of the babies with this condition are either stillborn or die immediately after being born. This condition occurs when all the four alpha globin genes are altered or missing.
Thalassemia minor
Thalassemia minor is a less severe form of thalassemia and is usually asymptomatic. Sometimes, symptoms like minor anemia may be found. The condition has been classified as either alpha or beta thalassemia minor. In alpha thalassemia minor, both the genes are missing while in beta thalassemia minor, only single gene is missing. Lack of symptoms usually makes thalassemia minor difficult to detect. It is important to get tested if one of the parents or a relative has some form of the disease.
Common Symptoms of Thalassemia
The symptoms of thalassemia differ according to the type of thalassemia. In case of infants with beta thalassemia, the symptoms do not appear until the age of 6 months because they have a different type of hemoglobin, called fetal hemoglobin. Since after the age of 6 months normal hemoglobin replaces the fetal hemoglobin, symptoms begin to appear. The main symptoms include:
- Frequent infections
- Pain in the chest
- Cramps in legs
- Pale skin
- Jaundice
- Skeletal deformities since the body try to produce more bone marrow.
- Dizziness
- Delayed growth
- Shortness of breath
- Excessive fatigue and drowsiness
- Head aches
- Cold feet and hands
- Rapid heart beat
- Poor feeding
Patients suffering from hemoglobin H usually have symptoms like gall stones and enlarged spleen. Sometimes there is excess iron in the body due to which body tries to compensate by absorbing more iron. This excessive iron can damage the spleen, heart, and liver. Excess iron gets accumulated in the body from blood transfusions also. If the thalassemia is not treated properly, its complications may result in organ failure.
What are the Causes of Thalassemia?
The anemia is due to excessive destruction of the RBCs caused by a genetic defect that decreases the red blood cell survival. Thalassemias are hereditary disorders and therefore get inherited from parents to children through genes. People who inherit the abnormal hemoglobin genes from one parent but normal genes from the other are called as carriers. Carriers usually show no signs of illness other than a mild anemia, but they carry the defective gene. Normal hemoglobin A, carries four protein chains—two alpha globin and two beta globin. The two major types of thalassemia, alpha and beta thalassemia are named after genetic defects in these protein chains. These two types of thalassemia can affect both males and females.
Beta thalassemia occurs if one or both genes producing the beta globin protein are altered. The severity of beta thalassemia depends on the number of affected genes. When both genes are affected it results in thalassemia major and severe anemia.
Alpha thalassemia occurs if one or two of the four genes which produce alpha globin are affected. If 3 genes are affected, it results in hemoglobin H disease and if all the genes are defective, it results in a severe form of alpha thalassemia called hydrops fetalis. This is due to this defect that such babies rarely survive.
Risk Factors for Thalassemia
Some factors which increase the risk of thalassemia include:
Family history of thalassemia
Thalassemia is inherited from parents to children through mutated hemoglobin genes. If a person has a family history of thalassemia, he has an increased risk of the condition.
Certain ancestry
It has been found that thalassemia occurs more in the African-Americans and in people of Mediterranean and Southeast Asian ancestry. Therefore they are considered at high risk.
Complications of Thalassemia
Some of the major complications of thalassemia include:
Iron Overload
People with thalassemia have too much iron in their bodies, either due to the disease or from frequent blood transfusions. This excessive iron can damage heart, liver and endocrine system.
Infection
A person with thalassemia is at an increased risk of infections, especially if his spleen has been removed. Severe cases of thalassemia result in the following complications:
Bone Deformities
Due to thalassemia, the bone marrow expands and the bones become wide. This results in abnormal bone structures, especially in the face and skull. Bone marrow expansion also makes bones thin and brittle and thereby increases the chance of broken bones.
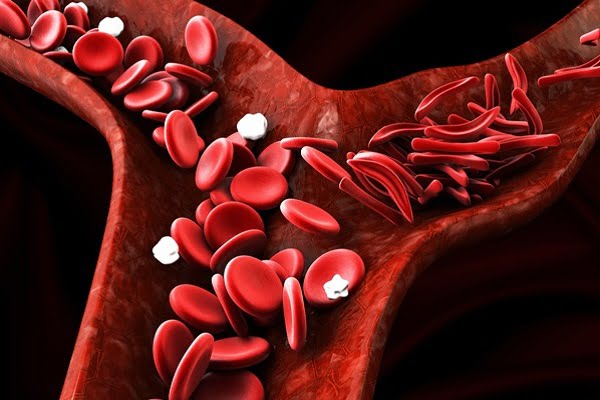
Enlarged Spleen (Splenomegaly)
Thalassemia often causes the destruction of a large number of red blood cells due to which spleen enlarges and works harder than normal. Enlarged spleen is called as splenomegaly, which can make anemia worse, and also reduces the life of transfused red blood cells. If spleen enlarges more, it is removed surgically (splenectomy).
Slowed Growth Rates
Thalassemia results in delayed puberty and anemia slows the child’s growth.
Heart problems
In most of the cases, thalassemias are often associated with heart problems like congestive heart failure and abnormal heart rhythms (arrhythmias).
What are the treatment options for thalassemia?
Usually, the treatment for thalassemia depends on the type and severity of the disease involved. However some common treatments include:
- Blood transfusions
- Bone marrow transplant
- Medications and Supplements
- Surgery for the removal of the spleen or gallbladder
- Chelation therapy for patients receiving blood transfusions
Prognosis of Thalassemia
The long-term outlook or prognosis for people with thalassemia usually depends on the type and severity of the condition. For example, severe thalassemia may result in early death due to heart failure, while less severe forms of thalassemia often do not decrease the lifespan. Fortunately, improved treatment options have resulted in increased survival rates and better quality of life for people affected with moderate to severe forms of thalassemia.