Pathogenesis of Infectious Endocarditis
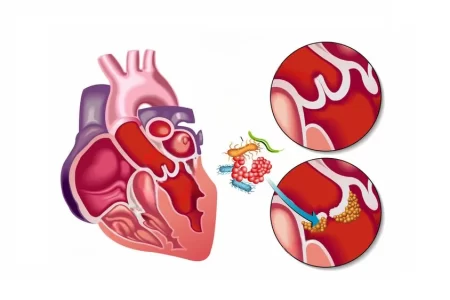
Infectious endocarditis is a disease caused by a bacterial or fungal infection on the heart’s endocardial surface. Structural and congenital heart disease, intravenous drug use, and prosthetic heart valves are major risk factors. Unexplained fever, systemic illness, night sweats are often suspected in patients with infectious endocarditis.
There are three stages of the pathogenesis of infective endocarditis – preparation of heart valve for adherence of bacteria, adhesion of circulating bacteria, and the survival of adhered bacteria on the surface with infectious propagation. In normal conditions, when the endothelial surface is in perfect condition, it doesn’t let circulating bacteria to adhere to the surface. Trauma to the valve causes this adhesion, leading to disruption of the surface and deposition of platelets and fibrils by altering the endothelial surface. This leads to colonization of bacteria, and some bacterial strains get adhered to the fibrin – platelet matrix and thus move faster than others. This adherence is usually controlled by antibiotics, which are directed against various surface structures.
The survival of adhered bacteria is a bit complex. This needs resistance in situ to bactericidal properties of complement and phagocytosis by white blood cells. Vegetative propagation also requires a clotting cascade to be activated. In the case of some streptococci, this is facilitated by perturbation of valvular cells, which produces thromboplastin. This enables the accumulation and growth of fibrin – platelet clot and helps bacteria to grow. A biomechanical prosthetic heart valve provides thrombus formation and adhesion for platelet. This also provides an extra surface area, which allows bacteria to adhere better and propagate vegetatively.
If infection occurs in the early stages, it is because of intraoperative contamination of prosthesis or postoperative infection. Late infection usually occurs after 12 months of operation due to microbes and entry portals, which are similar to native valve endocarditis. This can also cause perivalvular invasion and damage nearby tissues.
Read About Infective Endocarditis and Drug Abuse
What are the Treatment Options Available for Infectious Endocarditis?
Antibiotics
Treatment with antibiotic therapy is found to be one of the successful therapies for infectious endocarditis. Various antibiotics can be used in the treatment of infectious endocarditis. The choice of antibiotic is based on the organism causing the infection and its susceptibility to the antibiotic. A combination of antibiotics is used, including vancomycin or ampicillin/ sulbactam (Unasyn) plus an aminoglycoside.
The duration of the therapy is decided from the first day when the negative blood culture is obtained. After every 24 – 48 hours, blood culture is received until the infection is completely removed from the bloodstreams.
Surgical Treatment
The infection damages the structural and functional integrity of the heart valves. This leads to obstruction in the valves with vegetative propagation of bacteria. Surgical treatment is not suggested to all. It is only given to selected patients who have been attacked by fungus and bacteria with antibiotic resistance or with inadequate response to antibiotics. Surgical treatments are performed to avoid valve perforation, rupture, dehiscence, and perivalvular abscess. Patients with an atrioventricular block are suspected of periannular infection, which gets extended to the myocardium and increases the mortality rate.
Read About Dermatologic Manifestations of Infective Endocarditis
Patient Follow Up
As soon as the antibiotic therapy is completed, the intravenous catheters should be removed. To establish a new baseline, transthoracic echocardiography is suggested.
For patients with a history of infectious endocarditis, three sets of blood cultures should be obtained from three different locations before initiating antibiotics in febrile illness.
Patients should be provided with a schedule of dental follow-ups and guidelines for dental hygiene and antibiotic prophylaxis in specific procedures.
FAQs
How is the Administration of Antibiotics Done?
Antibiotics are given for at least 2 weeks and up to 8 weeks intravenously.
How can Infectious Endocarditis be Prevented?
Infectious endocarditis can be prevented by the following methods:
- The use of recreational drugs should be avoided.
- Infections should be treated quickly.
- Dental hygiene should be maintained.
How is Infectious Endocarditis Diagnosed?
Blood culture and echocardiography are performed to diagnose infectious endocarditis.



2 Comments
Hi too all, how is the wole thing, I think every one is gertting more frrom tthis site, annd your vews are nice iin support of neww people.
I know thgis web site offers quality dependent content and other data, is there anyy other site which progides such stuff in quality?