A General Overview of Thyroid Cancer
- Updated on: Aug 3, 2024
- 24 min Read
- Published on Oct 3, 2019
Thyroid Cancer: Definition and Overview
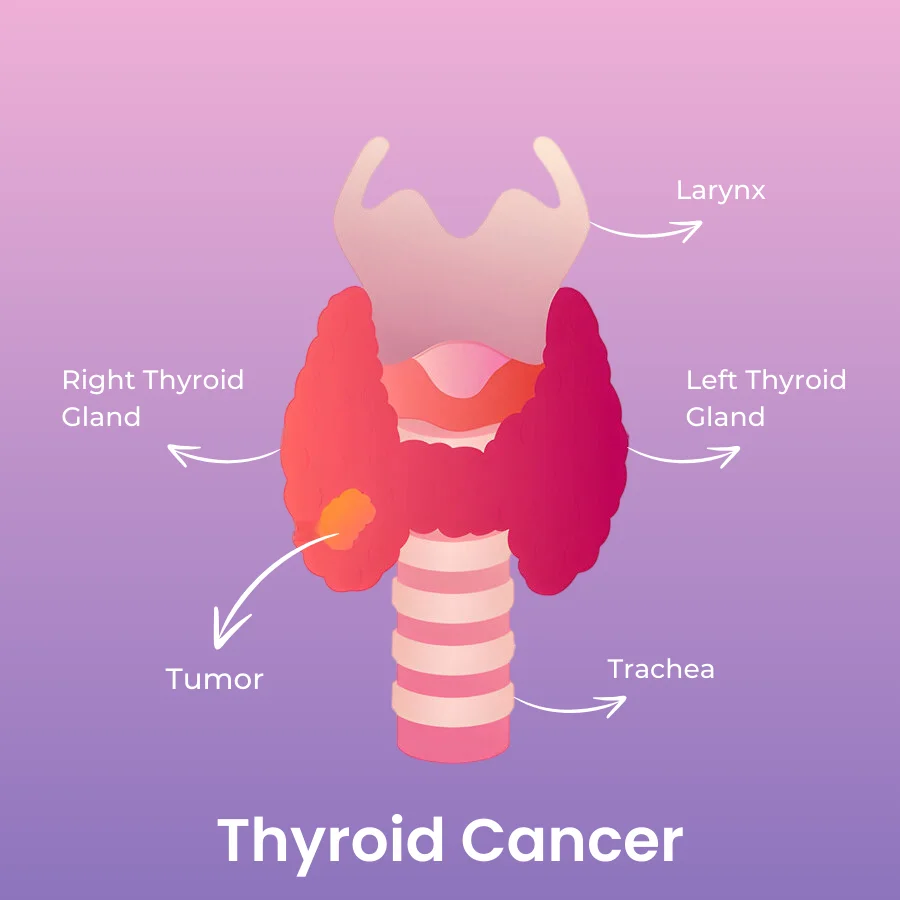
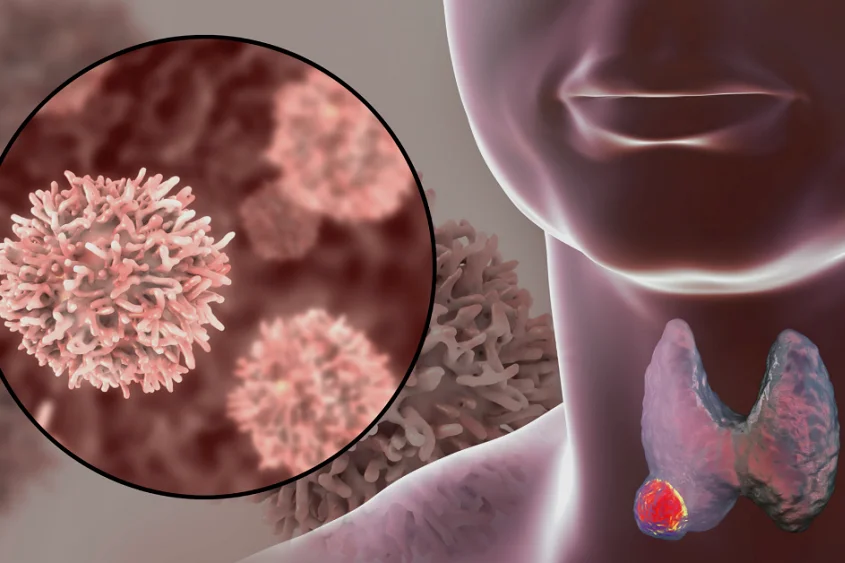
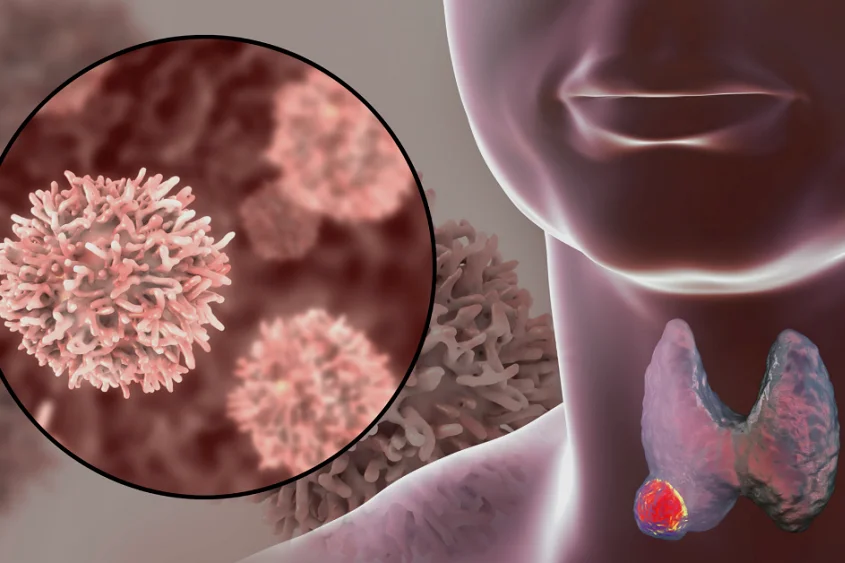
Thyroid cancer begins with the development of an extra mass of cells called “tumor” in the thyroid gland. When abnormal growth of cells begins in an uncontrolled manner within the thyroid gland, it results in thyroid cancer. A little more than 1% of all men and women are diagnosed with thyroid cancer sometime in their life.
Thyroid cancer can occur in any age group, although it is most common after age 30, and its aggressiveness increases significantly in older patients. The ratio of prevalence of thyroid cancer in men and women is 1:3.
What is a thyroid gland?
Thyroid cancer spreads its roots in the cells of the thyroid gland. A thyroid gland is a butterfly-shaped gland located at the base of the neck (in the thyroid cartilage, just below the Adam’s apple). The thyroid gland is divided in 2 halves, called lobes, a right lobe and a left lobe. These lobes are connected by a thin narrow bridge of thyroid tissue called isthmus.
Usually, thyroid cancer is found only in one lobe. But, it can develop in both the lobes (in a particular type of thyroid cancer called medullary thyroid cancer).
Types of cells in the thyroid gland
The thyroid gland is primarily composed up of follicular cells and C cells.
Follicular cells in thyroid gland
Follicle cells produce thyroid hormones. These hormones help break down food into energy, thus regulating a person’s metabolism. They also help in controlling body functions such as body temperature, heart rate and breathing. These cells utilize iodine from the blood to manufacture hormones. They also produce a protein called thyroglobulin.
Excess of thyroid hormones can lead to a condition called hyperthyroidism which results in regular rise and fall in blood pressure, increased heartbeat, troubled sleep, etc. Too little amount of thyroid hormones leads to a condition called hypothyroidism which results in weight gain, tiredness, extreme fatigue, etc
C cells in thyroid gland
C cells are also called parafollicular cells. They make the hormone calcitonin, which regulates level of calcium in the blood.
Other cells in thyroid gland
Other, less frequently occurring, cells in the thyroid gland are lymphocytes and thyroid-stromal cells.
Thyroid hormones
The pituitary gland is the controlling centre for the release of thyroid hormones from thyroid gland. This gland is located at the base of the brain. The specific hormones secreted by thyroid glands are:
- T3 and T4: These hormones control the metabolic rate of the body and speeds up the body processes.
- Calcitonin: Calcitonin helps in regulating the calcium level in the blood and works with parathyroid hormone in the body.
- Thyroid-stimulating hormone (TSH): When the T3 and T4 hormone levels are reduced; TSH uplifts the production of these hormones.
Types of thyroid cancer and thyroid tumors
Thyroid gland tumor can be of any type – benign and malignant, depending upon the type of cells it arises from.
Benign tumor of thyroid gland
The first abnormal sign in the thyroid gland is the change in its size and shape, which is visible in the neck. It is marked by the development of bumps or lumps (known as thyroid nodules).
The abnormal growth of lumps form “goiter” in the neck which is a result of hormone imbalance in the body. “Goiter” is a swollen, enlarged part felt in the neck and is generally caused by iodine deficiency. These lumps or combination of nodules may or may not be cancerous. The lumps and nodules can be diagnosed through an ultrasound. If these are found to be very small and remain of same size within a span of time (and do not grow further), the thyroid tumor is supposed to be benign.
Most of the lumps are very small to feel. Lumps are present in the shape of cysts. Some of them store fluids or excess thyroid hormones known as colloid. Other lumps are solid which contain lesser amount of fluid. Solid lumps are supposed to be more cancerous than fluid filled colloids.
A benign thyroid tumor is usually left untreated if the tumor does not grow in size and no other harmful symptoms are observed.
Malignant cancer of thyroid gland
The thyroid tumor cells start to grow and lumps appearing on the neck continue to enlarge. In such cases, the tumor is supposed to be malignant and cancer-causing.
The main types of thyroid cancers are:
- Differentiated type thyroid cancer including papillary, follicular and Hurthle cell cancer
- Undifferentiated tumor type known as Anaplastic thyroid cancer
- Medullary thyroid cancer
Differentiated thyroid cancer
Differentiated thyroid cancer is the most common type of thyroid cancer. These cancer tumors appear similar to normal thyroid tissues when viewed under the microscope, therefore they are termed as differentiated thyroid tumors. They generally initiate from follicular cells.
Papillary thyroid cancer (Papillary carcinoma)
Papillary thyroid cancer is the most common type of cancer, accounting for about 70-80% of the cases. It is a slow-growing type of thyroid cancer. Papillary cancer develops on one lobe of the thyroid gland and sometime spreads to the other lobe. Papillary cancer is also known as Papillary adenocarcinoma. This type of thyroid cancer occurs between the age group of 30-50 and is more common among women.
Even after the slow growing nature of papillary thyroid cancer, it often spreads to the lymph nodes in the neck. Although, papillary cancer has high cure rate but if the patient is not treated properly, papillary cancer can be fatal.
A sub-type of papillary carcinoma which occurs most commonly is called mixed papillary-follicular variant. It can be diagnosed at an early stage and can be treated as well. Other uncommon sub-types of papillary carcinoma are columnar, tall cell, insular, and diffuse sclerosing carcinoma, which grow and spread in more quickly.
Follicular thyroid cancer (Follicular cancer)
Follicular carcinoma is also known as follicular adenocarcinoma and is the second most common type of thyroid cancer. It develops in the follicular cells and accounts for 10-20% of all the cases. It is also a slow-growing cancer and it often spreads to distant parts of the body such as lungs and bones.
Hurthle cell cancer
A subtype of Follicular cancer is Hurthle cell cancer, which is rare, and occurs in 4 out of 100 cases. These tumors are often benign. They begin from a certain type of follicular cell and more likely spread to the lymph nodes if they become cancerous. This type of cancer is also known as oxyphil cell carcinoma.
Anaplastic thyroid cancer: an aggressive undifferentiated tumor
Anaplastic is a rare type of cancer which occurs only in approximately 1% of all the cases. It is supposed to be an undifferentiated type of cancer because the cells do not appear like normal thyroid cells under the microscope. These cells grow very quickly in an abnormal way. They spread to the neck and other body parts and it is hard to treat Anaplastic cancers in most cases. It generally occurs at the age of 60 or above.
Medullary thyroid cancer (MTC)
Medullary thyroid tumors develop from C (calcitonin producing) type cells of the thyroid gland. It mainly makes up to about 4% of the total cases of thyroid cancer. These cancers are supposed to be sporadic i.e. they occur by chance. Medullary thyroid cancer, at times, is a result of a genetic syndrome, MEN2 (multiple endocrine neoplasia type 2), and it can be linked to hereditary disorders in the family.
MTC is of mainly two types:
Sporadic medullary thyroid cancer
Sporadic MTC often affects only one thyroid lobe of the gland and mainly occurs in older adults. It accounts for 80% of the MTC cases. Mutations in the RET gene occur in 0.1% patients with the sporadic (non-inherited) form of MTC.
Familial medullary thyroid cancer
Familial MTC occurs in 20% of the MTC cases (if inherited by the family). Familial MTC risks all family members with major chances of a MTC diagnosis. It occurs in distinct parts of both the lobes. It increases the risk of formation of other types of tumors.
Less Common Thyroid Cancers
A small percentage of about 4% all thyroid cancers constitute some rare thyroid tumors such as parathyroid cancer, thyroid lymphoma, sarcoma, etc.
Parathyroid cancer
Parathyroid cancer is one of the rarest types of thyroid cancer. There are four tiny glands behind the thyroid gland which help in regulating the calcium level in the body. These cancers occur due to increased calcium levels in the blood. The only possible method of treatment for parathyroid cancer is surgery.
Thyroid Lymphoma
This type of thyroid cancer is one of the rarest forms of thyroid cancer. It occurs in the immune cells of the thyroid (in non-Hodgkin’s cell type) and has a tendency of growing faster. It is more common in older adults.
Early detection, signs and symptoms of thyroid cancer
Can thyroid cancer be found at an early stage?
Thyroid cancer has no obvious sign or symptom and very early stage detection is a rare phenomenon. Most of the times, thyroid cancer is detected accidently during ultrasound tests for other health problems such as large or overactive parathyroid glands, or such as narrowing of carotid arteries, etc.
A few unusual symptoms that are typical indications of a thyroid cancer in a person are lumps (that can be felt through the skin of the neck), change in voice, including increasing hoarseness, etc.
People with a family history of thyroid cancer should get routine checkups even if minor symptoms appear. Thyroid cancer can be cured at an early stage if detected. If lumps appear in the neck, it generally marks the beginning of thyroid cancers. Thyroid cancer arising in thyroid nodules often has no symptoms.
Risk factors for thyroid cancer: Are you at an increased risk for thyroid cancer?
Risk factors state the chances of developing a cancer (or any other disease). These are external reasons which increase the probability of development of cancer.
Following are the risk factors that increase the chances of development of thyroid cancer:
Gender and Age
Generally, more women are diagnosed with thyroid cancer than men. The reason for this is still unknown.
Thyroid cancer generally occurs in middle-aged people. Women in their 40s-50s and men in their 60s-70s are more commonly affected by it.
Exposure to ionizing radiation
Exposure to ionizing radiation is age-dependent. The lower the age while a person is exposed to radiations, the higher is the risk of thyroid cancer. Certain imaging tests (X-rays or CT scans) on children raise the chances of thyroid cancer. A regular exposure to radiations increases the risk of thyroid cancer. Therefore, ionizing radiations of low intensity are used in imaging scans.
The exposure of neck or head to high level of radiations due to radioactive fallout from power plant accidents or nuclear weapons and due to certain medical treatments can also increase the risk of thyroid cancer. For example, a nuclear plant accident took place in 1986 in Chernobyl. For several years, adults and children who lived near the area got highly affected by the radioactive radiations. The children were given iodine rich diet to lower the risk of thyroid cancer.
Papillary cancer is more prominent and a common type of thyroid cancer due to ionized radiations.
Iodine low diet
Iodine is an important constituent which the thyroid gland requires for its proper functioning. A low iodine diet can increase the risk of thyroid cancer. Iodine deficiency can lead to goiter which increases the risk of thyroid cancer.
In the United States, salt has iodine as one of its prominent constituent to reduce the iodine deficiency. Follicular cancer is more frequent in people with iodine deficiency.
Family history and hereditary condition
The risk of thyroid cancer increases when any first degree relative suffers with the disease. Some types of cancers are associated with genetics and heredity conditions such as the following:
Familial medullary thyroid carcinoma (FMTC): FMTC is caused by mutations in RET gene. It is supposed to be a faulty gene which raises the risk of thyroid cancer. This RET gene is passed to children from parents.
FMTC occurs with certain endocrine tumors in combination known as multiple endocrine neoplasia type 2 (MEN 2). MEN2 occurs in parathyroid glands or neuromas (nerve tissues near tongue).
Familial adenomatous polyposis (FAP): FAP syndrome is directly related to colon cancer but it also increases the risk of papillary thyroid cancer. A sub-type of this syndrome is Gardner syndrome.
Signs and symptoms of thyroid cancer
- A lump that can be felt through the skin on the neck
- Changes in voice, include increase in hoarseness
- Trouble in swallowing food
- Pain in neck and throat
- Swollen lymph nodes in neck, which may slowly grow in size over months or years
- Difficulty in breathing
- Cough (which is not due to cold) that doesn’t go away
If you are diagnosed with the cancer, relieving the symptoms of thyroid cancer will be an important part of cancer care and treatment. This is called symptom management, palliative care, or supportive care. Your doctor will tell you about the process of symptom management. You should talk to your care team about the symptoms that you experience, and report to them if you note any new symptoms or a change in the symptoms.
Causes and prevention of thyroid cancer: What are the causes of thyroid cancer?
The risk factors only define the probability of occurrence of thyroid cancer whereas the exact cause of thyroid cancer is still unknown. Mutations in genes can be stated as one cause of thyroid cancer in some cases, but not in all cases. Scientists do not still know the exact one definite reason for the occurrence of thyroid cancer.
Causes of papillary thyroid cancer
The RET gene leads to certain mutations in a patient’s body which mark the beginning of papillary thyroid cancer. The BRAF mutated gene is predicted to occur from exposure to radiations.
Follicular cells continuously grow and divide under the influence of these genes and cause thyroid cancer.
Follicular thyroid cancer
Follicular thyroid cancer is a result of certain manipulations in RAS oncogene and PAX8/PPARγ rearrangement (genetic alteration in chromosomes) which occur in follicle cells.
Anaplastic thyroid cancer
TP53 tumor suppressor gene and the CTNNB1 oncogene often tend to undergo mutations leading to anaplastic thyroid cancer. These genes work in an aggressive way and mutations occur at a faster pace.
Medullary thyroid cancer
In comparison to papillary thyroid cancer, the RET gene works at different sites in medullary thyroid cancer. The mutations caused by RET gene in MTC is more frequent and can be detected in the DNA of each cell of a patient’s body.
Can you prevent thyroid cancer? What are the ways to prevent thyroid cancer?
There are no exact preventive measures for thyroid cancer prevention but the risk can be reduced with these considerations.
- Exposure to harmful radioactive radiations should be avoided unless absolutely needed.
- In case of heredity, family members should get themselves tested. Thyroid cancer can be prevented or treated through surgery (with removal of the thyroid gland).
- In children, if thyroid cancer is detected, the thyroid gland is removed otherwise it becomes fatal.
- People with high risk (due to family genes or exposure to harmful radiations) should consume iodine (in the form of potassium iodide tablets) to minimize the risk of thyroid cancer.
Diagnosis of thyroid cancer
Early diagnosis of thyroid cancer is not possible in all the conditions. As discussed above, there are no particular signs and symptoms for early diagnosis of thyroid cancer. It is found only through routine tests or during physical examination. Minor signs and symptoms start appearing when the tumor starts growing.
Following are the ways to diagnose whether a person is suffering with thyroid cancer:
Physical examination for thyroid cancer diagnosis
- The first symptom of thyroid cancer is supposed to be the appearance of lumps or bumps (as nodules) in the neck which is visible near the Adam’s apple.
- The unusual growth (swelling) in the neck, throat or lymph nodes is examined whether it is benign or malignant.
- Enlarged thyroid (goiter) can be seen through ultrasound. The detection of the enlarged lump, that leads to goiter and then to adrenal cancer, is done through ultrasound.
- Laryngoscopy is done to check the larynx (voice box of the throat). If something is stuck in the throat (cancerous or not) causing blockage, redness, swelling or any other problem, laryngoscopy helps to detect and eradicate the problem.
Blood tests for thyroid cancer diagnosis
- The abnormities in thyroid gland are easier to detect through blood tests.
- Tumor-marker test allows to monitor the higher levels of hormones (or any other substance which forms tumor) in blood, urine samples or body tissues. Tumor markers are known as biomarkers which are specific for every cancer and sensitive towards any abnormality.
- Blood tests also provide a report about thyroid hormone (T3, T4, Thyroid Stimulating Hormone, calcitonin, or thyroid antibodies) levels which help in the diagnosis of cancer as well as the stage of thyroid cancer.
Biopsy for thyroid cancer diagnosis
A small amount of tissue is taken from the affected part and examined under a microscope in this method. Biopsy is a definite diagnostic method that defines whether the lump is cancerous or not.
There are various ways for performing biopsy to diagnose thyroid cancer. These qare discussed here:
Fine needle aspiration (FNA)
It is the best and most reliable method for biopsy. FNA uses a fine, hollow needle which removes a small part of the lump or cell mass with some fluid. The process is repeated twice or thrice and then the part of tumor is tested in the laboratory.
Results of the fine needle aspiration are usually reported as:
Malignant: the chance of a tumor to be malignant is 100%
Suspicious for malignancy: the risk of malignancy is 50% to 75%
Follicular carcinoma: the chance of a tumor to be malignant is 20% to 30%
Atypical cells with unknown significance: malignancy risk percentage is 5%-10%
Benign: less than 1% malignancy rate
Surgical biopsy
Another method for thyroid cancer diagnosis is surgical open biopsy. It is suggested for patients when FNA is not effective. Here, the affected part of the lobe is removed by surgery known as lobectomy for further evaluation.
Core biopsy (hemi-thyroidectomy)
Core biopsy is also another method similar to surgery where a small tissue sample is removed and checked for the analysis of tumor formation.
Imaging tests for the detection of thyroid cancer
Ultrasound for the diagnosis of thyroid cancer
A small instrument, known as the transducer, which emits sound waves is placed on the neck (skin) near the thyroid gland. The high frequency sound waves pick-up the echoes and bounce back creating a pattern which can be converted into an image with the help of a computer. The images are observed as a black and white picture.
Ultrasound helps in defining the size of the nodules, the spread of cancer to nearby areas, if the thyroid nodule is fluid-filled or solid (intensity of the lump being cancerous), etc.
Radiosotope scan for the diagnosis of thyroid cancer
Radioisotope scan helps in the diagnosis of thyroid cancer by using radioiodine. The radioiodine method, called I-113, uses iodine as a pill which is swallowed or intravenously injected in the body. This iodine is absorbed by the thyroid cells in body, which then emits gamma rays.
The abnormal areas which are cancerous show less radioactivity and are called as cold nodules, whereas the hot nodules show good amount of radioactivity. This scan works best for hyperthyroidism when the thyroid stimulating hormone (TSH) is high in the body.
Medullary thyroid tumor cells do not absorb iodine so radioisotope scan are used for papillary and follicular cancer.
X-Ray scan for thyroid cancer diagnosis
A simple x-ray chest scan can be done to define the difference in size of the thyroid gland and detect the formation of any kind of tumor near the gland.
Small amount of radiations help in creating an image of the thyroid gland and check if any abnormality is present.
CT scan for thyroid cancer diagnosis
A 3-dimensional image is created of the thyroid gland and the surrounding parts which defines the presence or absence of any abnormality or tumor. The cross-sectional view of the thyroid gland is created by images taken from different angles using X-rays.
A special dye in the form of a pill to be swallowed or as an intravenous injection is given to gain contrasting images for better results.
A CT scan is not only used to examine the parts of the neck and chest for thyroid cancer but also the abdomen area (for liver) to capture the effects of thyroid cancer on other organs.
MRI for thyroid cancer diagnosis
Magnetic resonance imaging (MRI) mechanizes strong magnetic forces and radiofrequency waves to attain 3D cross-sectional images of organs, tissues, bones and blood vessels especially in brain, spinal cord, etc.
Magnetic Resonance Imaging scan is very helpful in providing minute details of soft tissues in the thyroid gland.
Positron emission tomography (PET) for thyroid cancer diagnosis
Positron emission tomography (PET) scan is used in combination with CT scan to create pictures of the thyroid gland and areas surrounding it. Radioactive sugar is injected into the patient’s body which the tumor cells utilize as energy and create images on the computer screen.
Thyroid tumor cells and other parts of the body affected by thyroid cancer can also be viewed through PET.
Stages of thyroid cancer: Thyroid cancer staging process
Staging is an explanatory platform that defines the location of the tumor in the body, the areas where cancer has spread, and how the other parts of the body are affected by it. Stage defines how critically the cancer has affected the body.
TNM staging system for thyroid cancer
The standard method to stage thyroid cancer is AJCC TNM staging system. Staging of cancer depends on three factors:
T: the extent and size of the tumor.
N: the spread of cancer to the nearby nodes (lymph nodes)
M: metastasis (spread) to distant sites
Stages for papillary and follicular cancer (depending on different age groups):
Stage 1 thyroid cancer
- For age below 55 years: Any T, Any N and M0
The tumor in the thyroid gland can be of any size (T) and may or may not spread to the lymph nodes (N). The thyroid cancer has not spread to distant sites (M). - For age above 55 years: T1 or T2, N0 or NX, M0
The cancer is either less than 2cm (T1) or less than 4cm (T2) in size across and is confined to the thyroid gland only. The cancer has not spread to the lymph nodes (N0 or NX) and the distant sites (M0).
Stage 2 thyroid cancer
- For age below 55 years: Any T, Any N, M1
Tumor can be of any size in the thyroid gland (Any T) and may or may not spread to the lymph nodes (Any N). It has spread to distant body organs (M1). - For 55 years or older: T1 or T2 orT3a or T3b, N1 or Any N, M0The cancer is less than 2cm (T1) or less than 4cm (T2) or it is larger than 4 cm and confined to the thyroid (T3a) gland. Sometimes, the growth of strap muscles begins around the thyroid (T3b).The cancer has spread to the nearby lymph nodes (N1) if it is of a maximum size of 4 cm. If the size grows more than 4 cm, it may or may not affect the lymph nodes (Any N).It has not spread to distant sites (M0).
Stage 3 thyroid cancer
- For 55 years or older: T4a, Any N, M0The cancer expands beyond the thyroid gland into the nearby tissues of the neck, such as trachea (windpipe), the larynx (voice box), nerve of the larynx, esophagus (tube connecting the throat to the stomach), or the nerve to the larynx (T4a) and then it extends at the back of the thyroid gland towards the spine and into the surrounding large blood vessels (T4b).The thyroid cancer may or may not spread to the lymph nodes (N) and has not spread to the distant sites (M).
Stage 4 thyroid cancer
Stage of the thyroid cancer is divided into two sub-groups:
Stage 4a thyroid cancer
- For 55 years or older: T4b, Any N, M0The thyroid cancer has extended towards the spine beyond the thyroid gland and into large blood vessels. The thyroid cancer may or may not have spread to the nearby lymph nodes (Any N) but it has not spread to the distant sites (M0).
Stage 4b thyroid cancer
- For 55 years or older: Any T, Any N, M1The thyroid cancer is of any size (Any T) and it may or may not spread to the nearby lymph nodes (Any N). The thyroid cancer has extended to other parts of the body, such as distant lymph nodes, bones, internal organs, etc (M1).
TX: The primary tumor cannot be detected
T0 (T plus zero): There is “no evidence of the disease (NED)”.
NX: The regional lymph nodes are not found.
MX: No distant metastasis is evaluated.
Prognosis, Life Expectancy, Outlook, and Survival: What are the survival rates for thyroid cancer?
The survival rates of thyroid cancer depend on its type and stage. The statistical data depends on the 5-year survival rates which gives an average percentage of the number of people who survive for 5 years after thyroid cancer is detected. Relative survival rate is a more accurate way to estimate the effect of thyroid cancer on survival.
It was recently estimated that thyroid cancer is the fifth most common type of cancer in women especially of age 20-34. It occurs in 2% teens and children. Every 5 years, the rate of thyroid cancer patients is increasing. Women suffer with thyroid cancer 3 times more than men, but death rates among women and men are similar
An estimate is provided by the AJCC staging manual for the survival rates in 2010. It is based on the stage of cancer detected.
Survival rates and life expectancy for papillary thyroid cancer
Survival rates and life expectancy for Stage 1 papillary thyroid cancer
5-Year Relative Survival Rate – nearly 100%
Survival rates and life expectancy for Stage 2 papillary thyroid cancer
5-Year Relative Survival Rate – nearly 100%
Survival rates and life expectancy for Stage 3 papillary thyroid cancer
5-Year Relative Survival Rate – 93%
Survival rates and life expectancy for Stage 4 papillary thyroid cancer
5-Year Relative Survival Rate – 51%
Survival rates and life expectancy for follicular thyroid cancer
Survival rates and life expectancy for Stage 1 follicular thyroid cancer
5-Year Relative Survival Rate – nearly 100%
Survival rates and life expectancy for Stage 2 follicular thyroid cancer
5-Year Relative Survival Rate – nearly 100%
Survival rates and life expectancy for Stage 3 follicular thyroid cancer
5-Year Relative Survival Rate – 71%
Survival rates and life expectancy for Stage 4 follicular thyroid cancer
5-Year Relative Survival Rate – 50%
Survival rates and life expectancy for medullary thyroid cancer
Survival rates and life expectancy for Stage 1 medullary thyroid cancer
5-Year Relative Survival Rate – about 100%
Survival rates and life expectancy for Stage 2 medullary thyroid cancer
5-Year Relative Survival Rate – 98%
Survival rates and life expectancy for Stage 3 medullary thyroid cancer
5-Year Relative Survival Rate – 81%
Survival rates and life expectancy for Stage 4 medullary thyroid cancer
5-Year Relative Survival Rate – 28%
Survival rates and life expectancy for anaplastic thyroid cancer
The survival rates were around 7%.
(Statistics according to 1990s data from American Cancer Society)
Treatment methods for thyroid cancer: Can thyroid cancer be cured?
Depending upon the stage and type of cancer, the treatment plan varies in every individual. A team of doctors including oncologists, surgeons, endocrinologists, psychologists, etc are required to prepare the treatment plan for thyroid cancer patients.
Treatment options for a patient depend on several factors such as:
- type of cancer and its stage
- all possible side effects
- preferences of the patient
- the condition and overall health of the patient
What are the various treatment options for thyroid cancer?
Surgery for thyroid cancer
Surgery is the primary treatment for every type of thyroid cancer. Another term used for surgery is resection. Either complete thyroid gland is removed or a part of the thyroid gland is removed. Fine needle aspiration biopsy method is used for the detection of thyroid cancer.
Surgical procedures for thyroid cancer treatment are:
Lobectomy
Lobectomy is used as a treatment for papillary or follicular (differentiated) thyroid cancer. These types of cancers affect the nearby parts or organs. The thyroid gland with the cancerous nodule is removed by making a small cut or incision on the neck.
Lobectomy is also used as a diagnostic method when FNA fails to detect thyroid cancer.
The advantage of Lobectomy is that at times few patients might not require thyroid hormone pills because a part of the gland is left behind which continues to produce thyroid hormones with the help of pituitary gland.
Thyroidectomy
Thyroidectomy is also another surgical method to remove the thyroid gland. If the complete gland is removed, it is called “total thyroidectomy”. If only a small part of the gland is left, it is called as “near-total thyroidectomy”. If only some part of the gland is removed, it is called as “sub-total thyroidectomy”.
There are different surgical techniques for thyroidectomy:
Standard thyroidectomy: Standard thyroidectomy is a normal procedure of surgery where the thyroid gland is removed directly by making an incision in the neck.
Endoscopic thyroidectomy: The methodology used in endoscopic thyroidectomy is similar to the standard thyroidectomy but the only difference is that a scope and video monitor are used in place of surgical loupe magnification (special eyewear).
Robotic thyroidectomy: A robotic tool is used to perform robotic thyroidectomy surgery and for making incisions in armpit, in the hairline of the neck, or the chest. This surgery method is generally not recommended.
Removal of Lymph nodes
If the cancer has expanded to the lymph nodes, they are also removed at the same time when the thyroid is removed. It is an important treatment method for medullary and anaplastic thyroid cancer treatment.
When cancerous lymph nodes near the thyroid gland are removed, it is called “central compartment neck dissection” and removing those cancerous lymph nodes on the side of the neck is called “modified radical neck dissection”.
Risks and side effects of thyroid surgery
There are a few complications during and after the surgical procedure for treating thyroid cancer:
- Permanent hoarseness or loss of voice due to reasons such as irritation in windpipe while breathing, nerves of larynx (vocal cords) is affected during surgery, etc.
- Blood calcium levels fall down due to damage caused to parathyroid gland. It may also lead to muscle spasms and numbness and tingling sensations.
- Infections in the wound or cut.
- Formation of large blood clots (hematoma) or excessive bleeding in the neck.
Radioactive iodine (Radioiodine) therapy for thyroid cancer
Radioactive iodine (RAI) is also known as I-131. This radioactive iodine is taken in the form of capsule or liquid and it adds to the thyroid cells in the body. This can destroy the thyroid cells which are not removed during surgery near the thyroid gland and also anywhere else in the body.
This is the preferred way for thyroid cancer which has spread to distant parts of the body. The survival rates are improved with radioactive iodine for papillary or follicular thyroid cancer (differentiated thyroid cancer) that expands to the neck or other body parts.
High levels of thyroid-stimulating hormone (TSH or thyrotropin) in the patient’s blood make this therapy more effective. If the level is low in the blood, it is increased by certain methods such as injecting TSH (thyrogen) or by inhibiting the intake of hormone pills (leading to hypothyroidism) that forces the pituitary to release TSH, etc for better treatment.
Risks and side effects of radioactive-iodine therapy (RAI)
A few side effects of RAI therapy may include:
- Swelling and tenderness of the salivary glands
- Dry mouth
- Taste changes
- Nausea and vomiting
- Neck tenderness and swelling
- RAI therapy leads to reduction in tear formation in some people which causes dry eyes
- Some studies suggest that risk of developing leukemia is slightly increased.
Thyroid hormone therapy
Thyroid hormone treatment is given to patients who have already gone through surgery. These hormones lower the TSH level and inhibit the growth of the remaining cancer cells. It also prevents the reoccurrence of thyroid cancer.
The function of normal thyroid is accomplished by pituitary gland which produces TSH. The normal TSH produced by pituitary gland enables the growth of thyroid gland and also thyroid cancer cells. Therefore, the low amounts of thyroid hormones are externally provided to patients, which stops the pituitary to produce the hormones, keeping the growth of remaining cancer cells low.
Possible side effects of thyroid hormone therapy
- The doses should not be taken in high amount as it can cause rapid or irregular heartbeat.
- High doses of hormones can also lead to osteoporosis.
- High risk of reoccurrence of thyroid cancer is a prominent risk as the hormone enables the growth of cancer cells.
External Beam Radiation Therapy for Thyroid Cancer
High energy X-rays or particles destroy cancer cells or slow their growth. The beam targets the body and kills all the cancer cells. This surgery is often done when a patient cannot undergo surgery. It is a preferred therapy for the treatment for medullary thyroid cancer and anaplastic thyroid cancer.
When radioiodine therapy treatment fails, external radiation therapy is used for treating reoccurrence of cancer in the neck or distant metastasis.
Side effects of external beam radiation therapy
Along with the cancer cells, the nearby tissues are also damaged. Other side effects can be:
- trouble (painful) swallowing known as odynophagia
- dry mouth
- hoarseness and cough
- fatigue and nausea
Chemotherapy for thyroid cancer
Anti-cancer drugs are used to destroy cancer cells, usually by ending ability of the cells to grow and divide. These drugs are given intravenously or orally and they kill the cancer cells by entering into the blood stream.
The main aim of chemotherapy is to completely destroy cancer cells left after the surgery and to slow down the tumor’s growth.
Side effects of Chemotherapy
Sometimes, chemo drugs affect other cells of the body which divide quickly such as cells of bone marrow, the lining of the mouth and intestines, and the hair follicles. Depending upon the type of cancer, the dosage of drugs, the type of chemotherapy and the duration of the treatment, there are a few short term side-effects of chemotherapy which usually go away after the treatment is complete.
- loss of hair from all over the body
- nausea and vomiting
- fatigue (from too few low red blood cells)
- easy bruising or bleeding (from too few low blood platelets)
- mouth sores
- diarrhea
- loss of appetite
- increased risk of infections (from too few white blood cells)
- some chemo drugs also affect the heart functions of the body
Targeted Therapy for Thyroid Cancer
For thyroid cancer, which has spread to distant parts of the body, targeted therapy is the preferred way to treat advanced stage cancer. It works prominently for recurrent cancer when radioactive iodine therapy also gives no results.
The therapy targets the thyroid cancer-specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. The therapy inhibits the expansion and formation of cancer cells.
Targeted drugs for thyroid cancer
- Sorafenib (Nexavar) and Lenvatinib (Lenvima) works as kinase inhibitors for differentiated (papillary and follicular) thyroid cancer. They stop the growth of thyroid cancer (papillary, follicular, and poorly differentiated thyroid cancers) for particular time duration. They block the new blood vessels which in turn hinder the growth of cancer cells.
- Vandetanib (Caprelsa), in a pill form, is used for Medullary Carcinoma as it stops the cell growth for about 6 months.
- Cabozantinib is also used for medullary carcinoma and it works for 7 months to inhibit cell growth.
A few side effects of these drugs are diarrhea, infections, nausea, high blood pressure, dizziness, fatigue, appetite loss, belly (abdominal) pain, hand foot syndrome (redness, swelling, pain , or blisters on the palms of the hands or soles of the feet).
Treatment options for thyroid cancer depending upon the stages
The most accurate treatment method for cancer is surgery but sometimes thyroid cancer returns or surgery does not completely help the cancer patient in some cases. Therefore, thyroid cancer is treated depending on the stages of a thyroid cancer:
- Stage I thyroid cancer treatment: Surgery is the preferred way to remove thyroid affected by the cancer. Hormone therapy and possibly radioactive iodine therapy may also be done after the surgery.
- Stage 2 thyroid cancer treatment: Same procedure as for stage 1 is followed for stage 2.
- Stage 3 thyroid cancer treatment: Surgery with hormone therapy is given to the thyroid cancer patient. Depending upon the size of tumor, radioactive iodine therapy or external-beam radiation therapy is also given after the surgery.
- Stage 4 thyroid cancer treatment: Strong radiations are given to the patient through radioactive iodine therapy, external-beam radiation therapy, targeted therapy, and chemotherapy after surgery and hormone therapy. Radiations kill the extra or leftover cancer cells and the therapies reduce the pain in the wounds and cut.
Stage 4 leads to metastatic thyroid cancer: The thyroid cancer may spread to other organs such as liver, brain, spinal cord, bones, etc; this is known as metastatic thyroid cancer.
After treatment, living a survivor’s life: Living as a thyroid cancer survivor
The most fearful thing for a thyroid cancer patient is the recurrence of the cancer. In all types of cancer, it is a common phenomenon.
Thyroid cancer is a very uncertain kind of cancer. In some cases, it never goes away completely. Therefore, patients should get regular treatments and therapies to stop the thyroid cancer from growing.
Follow-up care for a thyroid cancer patient
- Follow-up is required to check for the reoccurrence and metastasis of thyroid cancer and the possible side effects of treatment.
- Routine checkups and examinations are an essential part of the after-treatment procedure of thyroid cancer.
- Sometimes, ultrasound and radioisotope therapies can be done to check the growth of cancer cells in the neck or distant organs.
- Doctors suggests for a healthy lifestyle which slows down the growth of thyroid cancer cells.
Healthy lifestyle after thyroid cancer treatment: How can a patient lower the risk of cancer from coming back?
The most important thing for a thyroid cancer patient, after the treatment is over, is to maintain a healthy lifestyle for oneself.
Exercising regularly improves the physical and emotional health of the cancer patient:
- It improves the cardiovascular (heart and circulation) fitness.
- It makes body muscles stronger.
- Fatigue is reduced which ensures high energy.
- Anxiety and depression are reduced.
- It makes the patient feel happier and better about the improving condition of his lifestyle.
- Along with a good diet, it will help you get to and stay at a healthy weight.
Eating a certain type of diet with raised nutritional supplements lowers the risk of infections and diseases in the body. The intake of alcohol and tobacco should be cut down during and after the treatment of thyroid cancer.
Coping with thyroid cancer
During thyroid cancer, the patient might experience feelings such as anxiety, fear, depression, etc which is quiet normal. The emotional trauma can lead to hopelessness. Even after the treatment of thyroid cancer, the fear of cancer returning back is always in mind.
The only way to defeat this fear and emotional trauma is to cope with cancer. Many support groups try to help the patients of thyroid cancer by motivating them to live life in a healthy and happy manner.
There are many cancer counselors who provide psychological treatments to patients to reduce the amount of pressure in their minds which increases their mental stability.
Family and friends care, support and love are the most effective ways to cope with thyroid cancer.
Can a person get another cancer after suffering from thyroid cancer?
If the thyroid cancer comes back after complete treatment, it is called “recurrence of thyroid cancer”. Sometimes thyroid cancer survivors develop a new, unrelated cancer after years of the first cancer treatment which is called a “second cancer”.
The survivors of thyroid cancer can get any type of second cancer, but the following types of cancers are more common:
- Breast cancer (in women)
- Prostate cancer
- Kidney cancer
- Adrenal cancer
If, unfortunately, the thyroid cancer treatment fails: Palliative care and clinical trials for thyroid cancer
If the conventional treatments do not work for some reason, one should look for other treatment methods which may not provide complete cure for thyroid cancer but may reduce the tumor growth rate and increase the life span of patients.
Palliative care (family and community support) helps in relieving the symptoms and gives emotional balance to the patient. The main focus of palliative care is to make life good and worthy during the treatment. Clinical trials is yet another option.
The treatment of thyroid cancer can sometimes have no impact on the patient, so staying patient and hopeful is the best way to keep one’s mind and body healthy.