About Stargardt Disease (Stargardt’s Macular Dystrophy)
- Updated on: Jul 12, 2024
- 6 min Read
- Published on Apr 21, 2021


What is Stargardt Disease (Stargardt’s macular dystrophy)?
Stargardt eye disease is a form of inherited juvenile macular degeneration. The disease leads to progressive vision loss due to the death of photoreceptor cells in the central portion of the retina called the macula.
The retina is a delicate layer of tissue that lines the back inside wall of the eye. It is located near the optic nerve. Retina is a light-sensing tissue and receives light that the lens has focused, convert the light into neural signals, and send these signals to the brain for recognition of images.
The disease generally causes loss of vision during childhood or adolescence. There are some forms though, where vision loss does not occur until later in adulthood.
Stargardt disease is also called Stargardt macular dystrophy, juvenile macular degeneration, or fundus flavimaculatus.
Stargardt disease prevalence
The estimated prevalence of Stargardt disease is 1 in 8,000 to 10,000 individuals.
See also: Age-related macular degeneration
What are the symptoms of Stargardt disease?
The main symptom of is Stargardt disease is loss of visual acuity that cannot be corrected with glasses. As a result, there is a loss in the ability to see fine details such as when reading or seeing distant objects.
Symptoms generally develop before age 20. These may include:
- blurriness
- loss of depth perception
- wavy vision
- blind spots
- sensitivity to glare
- some people develop color blindness later in the disease
- impaired colour vision
- difficulty in adapting to dim lighting – this is called delayed dark adaptation
- eyes may be more sensitive to bright light
The symptoms may significantly different among individuals. The progression of symptoms in Stargardt disease is different for each individual. People who have an early onset of the disease usually experience more rapid vision loss.
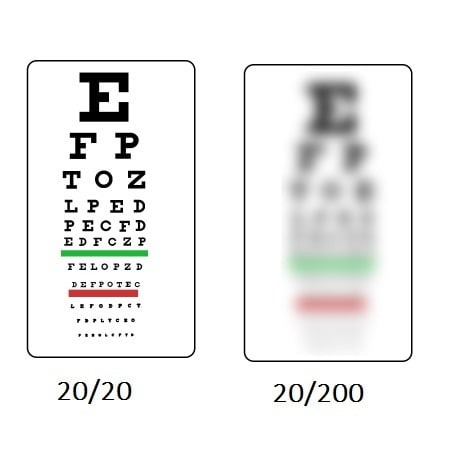
Vision loss may decrease slowly in the beginning, but usually worsens rapidly later. In most cases, people with Stargardt disease end up with 20/200 vision or even worse. Peripheral vision is generally less affected than fine, central vision in these people.
 What does someone with Stargardt disease see? Does Stargardt disease lead to blindness?
What does someone with Stargardt disease see? Does Stargardt disease lead to blindness?
People with Stargardt disease end up with 20/200 vision or even worse in most cases. This is legally what one would call someone a blind. To be considered legally blind, your vision needs to be 20/200 or worse. This means you can read something at 20 feet about as well as someone with normal vision could read it at 200 feet. However, it is rare for people with the disease to become completely blind.
When your vision is 20/200 or worse, the world looks entirely different to the person. Here is the comparison.
What causes Stargardt disease? Is it an inherited disease?
Stargardt disease is an inherited disease that is passed along to children when both parents carry mutations of a gene associated with vitamin A processing in the eye. Parents can carry recessive genetic traits that are responsible for Stargardt’s, even though they themselves may not have the disease.
Mutations in a gene called ABCA4 are the most common cause of Stargardt disease. This gene makes a protein that normally clears away vitamin A byproducts inside photoreceptors of the retina. Cells that lack the ABCA4 protein aggregate lipofuscin, a fatty substance that forms yellowish flecks. As the amount of lipofuscin increases in and around the macula, vision loss occurs. At one point of time, these fatty deposits cause the death of photoreceptors leading to almost complete vision loss.
Our retina contains light-sensing cells called photoreceptors. There are two types of photoreceptors: rods and cones. Both cones and rods are damaged in Stargardt disease. But, cones are more strongly damaged than rods.
Inheriting Stargardt disease: Genetics of Stargardt disease
Genes are grouped together on chromosomes. One copy of each chromosome is passed by a parent through egg and sperm cells.
In autosomal recessive inheritance pattern of a disease, it requires two copies of the mutant gene to cause the disease. An individual who has one copy of a recessive gene mutation is known as a carrier. When two carriers have a child, these possibilities arise:
- there is a 1 in 4 chance of a child born with the disease
- there is a 1 in 2 chance of a child born as a carrier of the disease
- there is a 1 in 4 chance of a child born such that he or she neither has the disease nor is a carrier
In autosomal dominant inheritance pattern of a disease, it requires only one copy of the mutant gene to cause the disease. If an affected parent with one dominant gene mutation has a child, there is a 1 in 2 chance that a child will inherit the disease.
Autosomal recessive mutations in the ABCA4 gene are responsible for most cases of Stargardt disease (about 95%). Other five percent of cases are caused by rare mutations in certain genes. Some of these mutations are autosomal dominant.
Diagnosis of Stargardt disease
An eye doctor can diagnose Stargardt disease by examining the retina. He or she can see Lipofuscin deposits as yellowish flecks in the macula clearly. These flecks generally extend outward from the macula and are clearly visible.
Methods used in the diagnosis of Stargardt disease:
Visual field testing
Visual fields testing method measures distribution and sensitivity of field of vision. A visual field test is an eye examination that is used to detect dysfunction in central and peripheral vision. The dysfunction may be caused by a variety of medical conditions such as glaucoma, stroke, brain tumors, retinal problems, or neurological deficits.
Visual field tests are done by eye specialists to detect blind spots and other visual field defects, which can be an early sign of many diseases and conditions of eye and brain.
Color Testing
These tests are used to detect loss of color vision, which usually occurs late in Stargardt disease.
Electroretinography (ERG)
The test measures electrical response of rods and cones to light. In this test, an electrode is placed on the cornea and light is flashed into the eye. The electrical responses are recorded on a monitor. If any abnormal patterns of light response are identified, it is indicative of Stargardt disease or any other diseases that involves degeneration of the retina.
Optical coherence tomography (OCT)
Optical coherence tomography (OCT) captures images by bouncing light waves off the living tissues. The patient is asked to place head on a chin rest. Light is then focused on the retina and detailed pictures deep within the retina are taken. These pictures are analyzed for any retinal abnormalities.
Fundus photo
A fundus photo is a picture of the retina. These photos may help in finding the presence of lipofuscin deposits. In this test, a special filter is used to detect lipofuscin. Lipofuscin is naturally fluorescent and glows in the dark when light of specific wavelength is passed through the eye.
See also: Retinal detachment: Causes, Symptoms, Diagnosis, and Treatment
Treatment of Stargardt disease: Is there a cure for Stargardt disease?
Currently, there is no treatment for Stargardt disease. But there are certain things that doctors recommend to prevent or slow down the progression of the disease. These are:
- Wear dark glasses and hats when out in bright light to reduce the buildup of lipofuscin
- Avoid cigarette smoking and second hand smoke
- UV blocking sunglasses are recommended for outdoors
- As found in some pre-clinical trials, high-dose vitamin A may increase lipofuscin accumulation and accelerate vision loss. Therefore, more than the recommended vitamin A should be avoided.
- Low-vision aids can be helpful for performing routine tasks
- Counseling and occupational therapies are also recommended as part of the treatment plan
Stargardt disease research advances
Stargardt disease stem cell therapy: How are stem cells used to treat Stargardt’s disease?
Stem cell-based therapies are being investigated in clinical trials. There is a promising evidence for Stargardt disease treatment using these therapies in these trials.
Stem cells are immature cells that can generate many mature cells in the body, including the photoreceptors that die in Stargardt disease. Stem cells can be obtained from embryonic tissues or adult tissues.
With recent advancements, retinal pigment epithelial (RPE) cells derived from human embryonic stem cells can be safely transplanted into the eyes of people with retinal degeneration.
Stargardt disease gene therapy: How successful it is for treating Stargardt disease?
Research published in Adv Exp Med Biol says that while the monogenic nature of many of the macular degeneration diseases makes them amenable to treatment with gene therapy, the ABCA4 cDNA is 6.8 kb and is thus too large for the AAV vectors which have been most successful for other ocular genes.
Some clinical trials are underway to treat patients with ABCA4-associated Startgardt’s disease (STGD1). With the development of novel technologies, effective therapies for ABCA4-associated diseases may be possible soon.
Oxford BioMedica is a gene therapy company based in the U.K. It has launched a Phase I/IIa clinical trial of gene therapy for people with Stargardt disease. The treatment employs the delivery of a corrective ABCA4 gene to the retina.
The company is now conducting a trial at Oregon Health and Science University, and is planning to begin a human study soon at Centre Hospitalier Nationale D’Opthalmologie des Quinze-Vingts in France. About 28 participants will be enrolled for this trial.
How quickly does vision fade in Stargardt disease (stargardt’s macular dystrophy)?
The progression of symptoms in Stargardt disease varies significantly. Visual acuity is the ability to distinguish among fine details and shapes. It may decrease slowly in the beginning, but accelerate later and then levels off.
In a study for people with Stargardt disease, it is found that when visual acuity of 20/40 is reached, there is a rapid progression of additional vision loss until it reaches 20/200. (Normal vision is 20/20. This means a person with 20/40 vision sees at 20 meters what someone with normal vision sees at 40 meters.)
By the age of 50, about 50% of people were found to have visual acuities of 20/200 or worse. And, almost everyone with Stargardt disease has a visual acuity in the range of 20/200 to 20/400.












