All You Should Know About Malaria
- Updated on: Dec 26, 2020
- 11 min Read
- Published on Dec 26, 2020

What is Malaria?
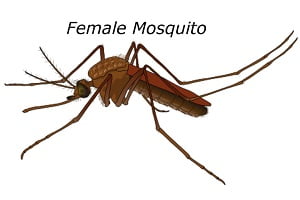
Malaria is a severe and life-threatening disease. Although it is preventable and curable, sometimes the complications associated with malaria can make it fatal. It is caused by a mosquito infecting Plasmodium parasite that commonly feeds on humans. It is transmitted and spread in the humans through the bite of an infected female Anopheles mosquito, also known as “malaria vectors.” When Anopheles mosquito bites you, the parasite is released into your bloodstream.
Once the mosquito has bitten you and parasites are released into your bloodstream, they travel to the liver, where they mature. After several days of maturation, the parasites enter the bloodstream and begin to infect your red blood cells. , the parasites inside the red blood cells multiply, causing the infected cells to burst open within 48 to 72 hours. The persistent infection of red blood cells by the parasites results in symptoms that occur in cycles that last two to three days at a time.
Patients who get malaria are typically very sick with high fevers, shaking chills, and flu-like illness. Humans are infected by these four main kinds of malaria parasites, which include:
Plasmodium falciparum Plasmodium vivax
Plasmodium ovale
Plasmodium malariae
Apart from these four plasmodium parasite species, another one is Plasmodium knowlesi that naturally infects macaques in Southeast Asia and infects humans. This causes a type of malaria that is transmitted from animal to human, also known as zoonotic malaria.
Out of these five species of plasmodium parasites, two parasites – Plasmodium falciparum and Plasmodium vivax poses the greatest threat.
P. falciparum is responsible for most malaria-related deaths globally, and it causes severe malaria infection if left untreated, usually leading to death. Geographically, it is the most prevalent malaria parasite on the African continent. In countries outside of sub-Saharan Africa, P. vivax is the dominant malaria parasite.
There are three important key aspects of the malaria life cycle:
The life cycle of malaria starts when the parasite is first carried by Anopheles mosquito.
The plasmodium parasite has multiple subspecies as listed above, each causing a different severity of symptoms. They also respond to different treatment options.
To grow, multiply and mature, these parasites first travel to a human’s liver, and from there, they reach the bloodstream where they infect and destroy red blood cells.
Where Is Malaria Found? How Common Is Malaria?
The presence of malaria is largely determined by climatic factors such as temperature, humidity, and rainfall of that geographic area. Malaria is typically transmitted and found in tropical and subtropical areas where climate is favourable for Anopheles mosquito to survive and multiply. The malaria parasites can complete their growth cycle in mosquitoes, known as the “extrinsic incubation period” in the tropical and subtropical climate.
Malaria is found in more than 100 countries, and according to The World Health Organization (WHO), in 2015, half of the world’s population were at risk of malaria. Some of the areas of the world where malaria is prevalent in dominant numbers include:
- Large areas of Africa and Asia
- Central and South America
- Haiti and the Dominican Republic
- Parts of the Middle East
- Some Pacific islands
WHO states that the African region carries a disproportionally high share of the global malaria burden. In 2016, this region alone was home to 90% of malaria cases and 91% of malaria deaths.
Globally, the World Health Organization estimates that 216 million clinical cases of malaria occurred in 2016, which was an increase of 5 million cases over 2015. In 2016, the toll of deaths due to malaria was 445,000. The majority of deaths were in children in African region.
The Centers for Disease Control and Prevention (CDC) report about 1,700 cases of malaria are diagnosed in the United States each year. In the USA, most malaria cases develop in people who travel to countries and immigrants returning from these parts of the world where malaria transmission is more common, including sub-Saharan Africa and South Asia.
Who Is at Risk to Get Malaria?
Risk factors which may increase your chances to get malaria include:
- Living in a country or traveling to a place where malaria is found
- Not taking preventive medicines while traveling to the areas where malaria is common
- Not taking preventative steps to avoid mosquito bites
Risk of getting malaria depends on the history of exposure to malaria, age, and pregnancy. People living in areas where malaria is common have developed partial immunity to malaria because of previous infections and rarely develop severe disease. But young children under the age of 5 who live in these areas and travelers to these areas are especially at risk for malaria because of lack of this acquired immunity.
What Causes Malaria? How Is Malaria Transmitted?
Malaria is caused by a bite from a female Anopheles mosquito infected with Plasmodium parasites. This parasite is passed into the human’s bloodstream when an infected mosquito bites them. Many different types of Plasmodia parasites are found in nature, but only five of them can infect and cause malaria in humans.
P. falciparum: Are major contributor to deaths from severe malaria, usually found in tropical and subtropical areas
P. vivax: Has a typical dormant stage that can cause a relapse of malaria and is found in Asia and Latin America
P. ovale: Mainly found in Africa and the Pacific islands
P. malariae: It is prevalent worldwide and can cause a chronic infection
P. knowlesi: Found throughout Southeast Asia and can rapidly progress from an uncomplicated case to a severe malaria infection
Humidity and ambient temperatures are the two important factors determining the successful development of the parasite within the mosquito.
You can get malaria if you come into contact with infected blood, blood transfusions, and the sharing of needles, but this is very rare. You can’t get malaria just by being near a person who has the disease. A mother infected with malaria parasite can also pass the disease to her baby at birth, known as congenital malaria.
Malaria is transmitted only by Anopheles mosquito. It doesn’t spread from person to person except during pregnancy, as stated earlier, and hence malaria is not considered a contagious disease. A number of steps are involved in the transmission of malaria, some of them include the following:
Infection of the Mosquito: When a mosquito bites and feeds on a person who has malaria, it becomes infected.
Transmission of Parasite to Uninfected Person: If you’re uninfected with malaria and you are the next person these mosquito bites, you can get infected by malaria parasites.
In the Liver: When an infected mosquito bites you, the parasite passes into your bloodstream from where it travels to your liver and lie dormant. The parasites mature during the dormant period. Some types of parasite can lie dormant for as long as a year.
Release Into the Bloodstream: After maturation, the parasite leaves the liver and is released back into the bloodstream, infecting your red blood cells. Generally, malaria symptoms are manifested at this stage.
Transmission to the Next Person: At this point in the cycle, if an uninfected mosquito bites you, it will become infected with your malaria parasites and can spread them to the next person it bites. This restarts the transmission cycle.
What is the Incubation Period for Malaria?
When you get infected with one of the Plasmodium parasites that cause malaria, you will not feel sick immediately; rather, you may feel normal from seven days to several years after infection. However, during this time, malaria parasites keep multiplying in your body. The period between your infection with the malaria parasite and the appearance of malaria symptoms is called the incubation period for malaria.
Plasmodium falciparum has a shorter incubation period of about 10-14 days, while Plasmodium malariae tends to have a longer incubation period. The incubation period for other species of plasmodium ranges between 10 to 17 days. However, the overall incubation period for malaria varies from 7 to 30 days. In some rare cases, they even can have an incubation period of about one year.
What Are the Symptoms of Malaria?
Malaria can generally begin with flu-like symptoms, and it has a wide spectrum of symptoms. It takes between 7 to 30 days after infection for symptoms to appear.
In the early stages, infections from all the species of plasmodium which infect humans are the same. You may experience no symptoms or very few and less severe symptoms if you are partially immune to malaria.
In regions where malaria is widespread, people may have the disease but have few or no symptoms. The severity of malaria can vary depending on your general health, the kind of malaria parasite you got infected with, and whether you still have your spleen.
Malaria has a very classical but rarely observed cycle of symptoms that lasts for 6-10 hours, which repeats itself every two or three days. The episode includes:
A cold stage – the sensation of cold and shivering.
A hot stage – symptoms like fever, headaches, vomiting, and seizures in young children.
A sweating stage – sweating followed by a return to normal temperature and tiredness.
This periodic pattern of malaria symptoms is due to the life cycle of malaria parasites as they reproduce, develop, and get released from the liver cells and red blood cells in the human body.
The symptoms of malaria are generally classified into uncomplicated and severe malaria.
Uncomplicated Malaria
This is diagnosed when the symptoms are present, but there is no sign of any vital organ failure, which may include:
- Fever
- Chills
- Headache
- Sweat.
- Fatigue
- Nausea and vomiting
- General weakness and body aches
- Enlarged spleen
- Mild jaundice
- Enlargement of the liver
- Increased respiratory rate
- Perspiration
Complicated or Severe Malaria
In severe malaria, there is clinical and laboratory evidence showing abnormalities and dysfunction of vital organs. In some cases, it can even lead to organ failure. Severe malaria should be treated aggressively and on an urgent basis. Various symptoms of severe malaria may include:
- Fever and chills
- Impaired consciousness
- Prostration, or adopting a prone position
- Multiple convulsions
- Deep breathing and respiratory distress
- Abnormal bleeding
- Clinical jaundice
- Anemia due to destruction of red blood cells
- Acute kidney failure
- Cardiovascular collapse
- Abnormalities in blood coagulation
- Unconsciousness, abnormal behavior, seizures, or confusion due to cerebral malaria
- Low blood sugar, especially in pregnant women after treatment with quinine
What Are the Complications of Malaria?
Malaria can be fatal, especially severe malaria, which can affect your body’s vital organ systems. The variety of malaria, which is common in tropical parts of Africa, has severe complications associated with it.
The effects of malaria and its associated complications are usually more severe in pregnant women, babies, young children, and the elderly. It is advised that pregnant women, in particular, should not travel to malaria-risk areas.
Most of the deaths caused by malaria are related to one or more of the following serious complications.
Cerebral Malaria
Cerebral malaria occurs when the parasite-filled blood cells block small blood vessels to your brain resulting in swelling of your brain, causing your brain damage. Cerebral malaria may impair consciousness, abnormal behavior, seizures, coma, or other neurologic abnormalities.
Breathing Problems
Pulmonary edema is a medical condition that is a result of the accumulation of fluid in your lungs. It can make breathing difficult for you. Malaria can also cause acute respiratory distress syndrome (ARDS), which is inflammation in the lungs resulting in oxygen exchange inhibition.
Organ Failure
Severe malaria, if left untreated, may cause your kidneys or liver to fail. In some rare cases, it may even cause your spleen to rupture. These all can be life-threatening and fatal conditions.
Anemia
Malaria parasites damage and destroy your red blood cells leading to severe anemia.
Low Blood Sugar
Severe malaria itself causes low blood sugar and also the quinine which is one of the most commonly used medications to combat malaria. The low sugar level in your blood can result in coma or death.
How Is Malaria Diagnosed? What Is the Rapid Diagnostic Test for Malaria?
Malaria symptoms can mimic many other diseases such as influenza or viral syndrome. Therefore it is important to inquire about recent travel history to an endemic area or other possible exposures.
The definite diagnosis of malaria is made by examining the blood of an infected patient under the microscope. It helps to determine the presence of the parasite as well as the type of parasite present in the blood smear with a specific stain. A blood smear test is the most widely performed and accepted test.
A rapid diagnostic test (RDT) is a quick way of establishing the diagnosis of malaria. It is a very fast method that can give the diagnosis in a few minutes. It detects the malaria infection by detecting specific malaria antigens in a patient’s blood. However, it is always recommended that a positive RDT test should be followed by a blood smear examination.
During RDT, a blood specimen collected from the patient is applied to the sample pad on the test card and certain reagents. After 15 minutes, the test card window is examined for specific bands, indicating whether the patient is infected with Plasmodium falciparum or one of the other 3 species of human malaria. A blood sample containing P. falciparum is used in the laboratory as a positive control.
RDT may not detect some infections with lower numbers of malaria parasites circulating in your bloodstream which can be a disadvantage. There is much debate on its ability to detect the 2 less common species of malaria, P. ovale and P. malariae. It is advisable to go for a blood smear test under microscopy for all the negative RDTs to confirm the result.
Treatment of Malaria
The key to malaria treatment is starting early, intending to eliminate the Plasmodium parasite from the patient’s bloodstream. Malaria can be cured, and early treatment can prevent the serious effects of malaria. A delay in treatment can cause malaria to be a severe, potentially fatal disease, especially the Plasmodium falciparum infection.
Patients without symptoms may get treated for malaria to reduce disease transmission risk in the surrounding population. In some instances, the medication prescribed may not clear the infection because of the parasite’s resistance to drugs. Your doctor may need to change medications altogether or use more than one medication to treat you in such conditions. Certain types of malaria, such as P. vivax and P. ovale, can live in your liver for an extended period reactivate later, causing a relapse of the infection. If you are found to have an infection with one of these parasites, you may be prescribed a second medication to prevent a relapse in the future.
The choice of drug and specific malaria treatment recommendation will depend on:
- The species (type) of the infecting parasite
- The area where you caught malaria
- The severity of your symptoms
- Your age
- Pregnancy
- Drug allergies
- Any other illnesses or conditions
- Other medications taken by the patient
For the treatment of uncomplicated malaria, the WHO recommends Artemisinin-based combination therapy (ACT).
Artemisinin is extracted from the plant Artemisia annua, commonly known as sweet wormwood. It has the ability to reduce the concentration of Plasmodium parasites in your bloodstream rapidly. In ACT, artemisinin is administered in combination with a partner drug. Artemisinin reduces the number of parasites within the first three days of infection, while the partner drugs eliminate the rest. However, malaria is becoming increasingly resistant to the effects of ACT, and for such cases, the treatment must comprise an effective partner drug.
There are different types of malaria medicine which your doctor can recommend according to your specific need. Most of them can be taken orally and, if not possible, then through an intravenous (IV) line. Medications used for treating malaria may include:
- Chloroquine
- Primaquine
- Artemether-lumefantrine
- Atovaquone-proguanil
- Mefloquine
- Artesunate
- Quinine
- Quinidine
- Doxycycline (used in combination with quinine)
- Clindamycin (used in combination with quinine)
- Sulfadoxine-pyrimethamine
Primaquine is specially used to treat forms of malaria parasites that may lay dormant in the liver for a longer period of time and help prevent malaria relapses caused by such parasites. It should not be taken by pregnant women or by people who are deficient in G6PD (glucose-6-phosphate dehydrogenase). The patient should not get this medication until a screening test confirms the exclusion of G6PD deficiency.
Is it Possible for Malaria to Comeback After Treatment? What Is the Prognosis and Long Term Outlook of Malaria?
P. vivax and P. ovale usually can hibernate in your liver and cause malaria relapse weeks or months after you are symptom-free. Malaria caused by these two parasites may recur at irregular intervals for up to 3 to 4 years, but medicine can prevent relapses. P. Malariae has a longer incubation period, and it can remain in the blood of an infected person for more than 30 years, usually without causing any symptoms.
The prognosis of malaria is very good if it is diagnosed and treated early. Malaria is responsible for over 400,000 deaths per year worldwide, where the majority of victims are young children from sub-Saharan Africa. Death is usually due to either lack of access to treatment or a lack of available treatment.
P. falciparum tends to have a higher share in being the cause of death due to malaria, causing the most complications if untreated. One of its complications is cerebral malaria, which has a 20% mortality rate even if treated.
Malaria patients, who are treated for the disease, typically have a good long-term outlook. The outlook may not be as good if complications arise as a result of malaria. For example, cerebral malaria, which causes swelling of the brain’s blood vessels, can result in brain damage. The patients with drug-resistant parasites may also have a poor long-term outlook. Chances of malaria recurrence in these patients are high, which may cause other complications.
How Can You Prevent Malaria?
Malaria can be prevented by taking antimalarial medicines and protecting yourself against mosquito bites. It is strongly recommended that people avoid travelling to areas where malaria is common, especially for young children and pregnant women. Malaria can often be avoided by the ABCD approach of malaria prevention, which refers to:
- Awareness of risk
- Bite prevention
- Check if you need to take malaria prevention tablets
- Diagnosis
You should first evaluate if malaria is a concern in the area you are travelling. To prevent malaria, chemo-prophylaxis is recommended; in that case, you should consult your doctor to know about the appropriate medicine.
You can prevent yourself from a mosquito bite by following these guidelines:
- You should stay inside a screened or air-conditioned room when it is dark outside.
- While in endemic areas, wear protective clothing such as long pants and long-sleeved shirts.
- Use insect repellent, particularly with DEET (N, N diethylmetatoluamide) on exposed skin. It should not be used in babies younger than two years of age.
- Use flying-insect spray indoors around sleeping areas.
- Use mosquito/bed nets soaked in or sprayed with an insecticide such as permethrin or deltamethrin.
Can You Get a Malaria Vaccine?
There is no approved vaccine for use in humans against malaria but research is underway to develop and make available an effective vaccine for malaria. Most of the efforts are being directed towards malaria caused by the parasite P. Falciparum because it causes the most serious form of malaria. RTS, S/ASO1 is the most advanced candidate as a viable vaccine against malaria. It has completed phase 3 of clinical trials and is being implemented on a pilot basis in several sub-Saharan countries with support from WHO.