Celiac Disease Diagnosis
- Updated on: Jun 27, 2024
- 3 min Read
By
- Published on Sep 26, 2019
How is celiac disease diagnosed?
Diagnosis of celiac disease can be difficult because of the following reasons:
- Many symptoms are similar to symptoms of other diseases like skin allergy, lactose intolerance and irritable bowel syndrome (IBS)
- Many people suffering from celiac disease may not have any symptoms at all
- Damage to intestine is a gradual process, it may take time to find out what actually is happening inside the body
- Celiac disease has a lot of symptoms and that too different for different people.
Diagnosis of celiac disease is done in a series of steps. These steps are performed one after the other. Your doctor may ask you to undergo through some tests and examinations in order to understand the disorder completely.
The steps of diagnosis are described below:
Family History
The doctor will ask about the patient’s family history, whether any of his relative or family members is celiac or not.
This is done in order to check the likelihood of the person of developing the disease. If any relative or family member is having celiac, the risk is bigger for the patient.
Physical Exam
During a physical exam, the doctor checks the patient physically, just by looking at the symptoms. The doctor often:
- Check for any stomach pain, bloating or swelling
- Use a stethoscope to analyze internal condition of the stomach
- Checks the body for any rash or malnutrition, which arises when the patient doesn’t get enough nutrients, minerals and proteins.
Dental Exam
Although dental enamel defects are caused by excess fluoride in drinking water, certain antibiotics or genetic diseases, and celiac disease are also a potential cause that should not be ignored. Following dental defects are very common in celiac patients especially among children
- Partial or complete loss of the enamel in permanent teeth
- Dental cavities
- Tooth Decay
- Sores inside mouth
- Whitish yellow spots on teeth
- Slow loss of baby teeth
It is estimated that dental defects range from 10 percent to 97 percent of the celiac patients. Sometimes dental enamel defect can be the only symptom of celiac disease among children. In order to clarify whether the dental defects indicate celiac disease or not, a dental check-up is necessary.
Skin biopsy
If the patient is suspected of having dermatitis herpetiformis (blistering skin condition), the doctor will perform a skin biopsy to check for the celiac disease.
For a skin biopsy, the doctor removes samples of skin tissues and examines them under a microscope. If the rash is of dermatitis herpetiformis, it will contain immunoglobulin A antibody.
The body (mainly intestine) produces this antibody when a patient feeds on a gluten-containing diet. The rash contains this antibody in a granular pattern. If skin biopsy confirms the presence of the antibody, the doctor may ask the patient to go through other blood tests.
Blood Tests
A sample of the patient’s blood is taken and is tested in order to diagnose the celiac disease. These tests are done to find out the antibodies that are produced by the body when the patient takes gluten.
Following blood tests are recommended for the suspected adults:
- Total immunoglobulin A (IgA)
- IgA tissue transglutaminase antibody (tTG)
Following blood tests are recommended for the suspected children:
- Total IgA
- IgA tTG
Suspected people are advised to continue eating gluten till the tests are done. Eliminating gluten from diet before tests may not give correct results. If the blood tests are negative and the doctor still suspects celiac disease, he may order some more tests to clarify.
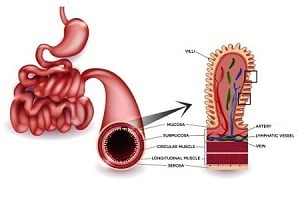
Intestinal Biopsy
If the blood tests are positive, the doctor may ask the patient to perform an intestinal biopsy. This confirms the diagnosis of celiac disease because this procedure explains the following:
- Whether the patient has celiac disease or not
- Whether the symptoms improve if gluten-free diet is introduced
- Whether the change in diet cause any other gastrointestinal disorder
How is intestinal biopsy done?
During an intestinal biopsy, a very thin tube with a small camera at the end is inserted into the mouth. When the tube reaches the small intestine, a tool is used to take four to six samples of tissue from the intestinal wall.
These tissues are then examined under the microscope. The patient should be on a gluten-containing diet till the biopsy is completed for accurate results.
Genetic Tests
If the above tests do not provide any clear result, the doctor may ask for genetic tests.
In order to develop celiac disease, the person must have either the HLA-DQ2 or HLA-DQ8 genes. If these gene variants are not present, the patient is very unlikely to have celiac disease. However, these variants alone are not enough to develop the disease.
Nearly 40 percent people have these genes, yet only some develop the disease. This is because an environmental trigger, like a stressful event, illness, pregnancy or any surgery is required to develop the disease.
Genetic testing is very much required for the relatives or family members of the people diagnosed with the disease.