Corneal Topography Mapping
- Updated on: Jun 27, 2024
- 5 min Read
- Published on Feb 13, 2020
What is Corneal Topography?
Corneal topography is a computer-assisted diagnostic procedure that provides information about the curvature and shape characteristics of the cornea.
It is a painless procedure used for creating the 3D mapping of the surface curvature of the cornea. The information obtained from corneal topography is very helpful for the perfection of contact lens fitting, analysis of corneal pathology, and illustration of corneal astigmatism.
One significant advantage of using corneal topography is that it can help in diagnosing various irregular eye conditions that cannot be found through conventional tests.
Corneal topography is found to help provide a detailed and visual description of the corneal shape and to diagnose the power. Analysis through corneal topography is very effective for patients and handy for physicians as well.
Corneal topography mapping is also used in placing contact lenses, for surgery such as LASIK or laser vision correction. This methodology is used in conjunction with other tests for determining the need for removal of corneal tissue with ablation patterns.
Technology to Perform Corneal Topography Mapping
Topographers can be small-cone or large-cone devices or systems. The primary technologies used in modern corneal topography are:
Placido Disc
Placido disc systems are categorized as small-cone or large-cone systems. These systems capture the reflected light and help in measuring the irregularities, curvature issues, certain foreign bodies, tear film disparities and some other characteristics of the anterior cornea.
It is also observed that small cones can collect more data points when compared to large cones. Small cones are able to present more rings as they cover more distance. This is why small cones are considered to be more accurate as compared to large cone systems.
More: Cross-linking eye surgery for keratoconus
More: Corneal transplant surgery
Scheimpflug and Scanning-slit topography
Initially, corneal topography was used to describe only the anterior surface of the cornea. Devices now can characterize both the anterior and posterior corneal surfaces, creating a three-dimensional map.
The benefit of using the Scheimpflug or scanning-slit topography system over the Placido disc is that it provides more information about the posterior cornea. The off-axis

light helps to capture measurements that are specific of the anterior and posterior surfaces of the cornea, and therefore allowing the system to test for global pachymetry. Pachymetry helps to measure the thickness of the cornea. This also helps to monitor characteristics such as corneal swelling while wearing contact lenses.
Figure: Corneal Topography Mapping at a Diagnostic Centre
(Image Credit: Wikimedia)
Techniques to Measure Corneal Topography
Corneal mapping is done to measure the curvature of the cornea. Main techniques and instruments are:
Keratometer
Also known as an ophthalmometer, this is the most commonly used instrument that helps to project an illuminated image onto a central area in the cornea.
A keratometer is used to measure the steepness of the cornea. It is found that keratometers measure only the central 3 mm of the cornea and topographers calculate 9 or 10mm of the cornea.
Keratoscope
A keratoscope reflects a series of concentric circular rings of the anterior corneal surface and the visual inspection of the shape and spacing of the concentric rings helps in providing a qualitative assessment of topography.
The limitation of this technique is that only a small percentage of the corneal curvature surface is a measure which also might not be entirely correct.
Computer-Assisted Photokeratoscopy
It is an alternative to keratometry or keratoscopy for measuring corneal curvature.
In this technique, sophisticated image analysis programs help to provide quantitative corneal topographic data.
How is Corneal Topography Mapping Done?
During corneal topography mapping, a doctor asks the patient to look into a bowl-shaped device that consists of illuminated concentric rings or “red rings”. A camera in the center of the device helps to capture the surface of the cornea.
Presently, latest technology uses tens of thousands of data points to read across the cornea in seconds. The height and the position of these points are used for mapping the state which is used by the physician to interpret the abnormality in the cornea.
Corneal topographic information can be represented through:
Use of Refractive corneal power maps
These maps help to measure spherical aberrations through ray-tracing for accurate presentation of corneal power.
Use of Instantaneous radius of curvature power maps
This is a very sensitive scheme and is mainly used to optimize the transition zone in the development of laser refractive surgery algorithms. The transition zone develops the “red ring” or spherical curvature.
Corneal elevation maps
These maps are obtained directly with fluorescein profilometry or with the scanning slit technology or from Placido disk topographers.
Corneal elevation display mapping helps in determining the best lens design to fit on an irregular cornea (between a corneal or scleral gas permeable lens).
Types of Corneal Topography Maps
Relevant information about the cornea condition is determined through different types of corneal topography maps.
Axial Display Mapping
Axial display maps are best recommended for an early and quick overview to check the corneal power.
These maps are considered to be “not so accurate” or misleading. The algorithm used in these maps allows assuming that a spherical surface and the cornea become more aspheric in the periphery and this leads to inaccuracy in outside edges. This can be a limitation in several cases.
Tangential Display Mapping
Tangential display maps are known to be sensitive maps that help to measure the most accurate power and curvature at individual points on the cornea.
Tangential maps are considered to be beneficial in orthokeratology (also known as ortho-k) to evaluate the shape of the peripheral cornea (either distorted or spherical). Any changes caused due to topographic abnormality of the cornea from contact lens wear can be caught up in tangential display as this is a highly sensitive mapping type.
Refractive Power Mapping
Refractive power maps help in interpreting the quality of vision through the corneal surface. These maps help in diagnosing how better a patient can see specifically due to the contribution of the corneal surface to visual acuity and in determining the effect.
These refractive power maps are less frequently used as they do not provide much information on curvature or size and shape of the corneal surface.
Elevation Display Mapping
Elevation display maps help in determining 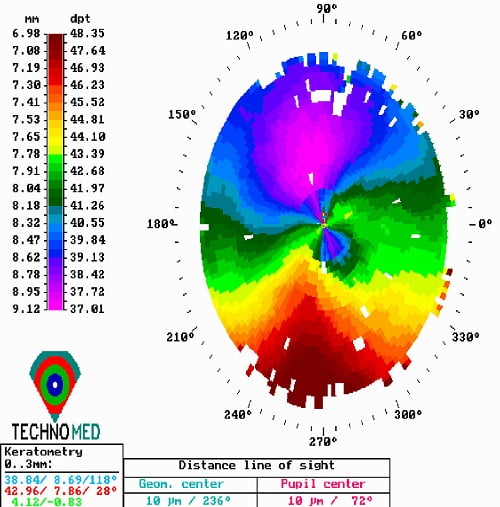 the best lens design to fit on an irregular cornea. The elevation display map helps in the management of orthokeratology as it allows in determining if the corneal shape is regular enough to support an ortho-k lens or not. This will be helpful in defining whether to use single-axis lens or a dual-axis lens by the ophthalmologist.
the best lens design to fit on an irregular cornea. The elevation display map helps in the management of orthokeratology as it allows in determining if the corneal shape is regular enough to support an ortho-k lens or not. This will be helpful in defining whether to use single-axis lens or a dual-axis lens by the ophthalmologist.
Figure: Result of Corneal Topography Examination.
(Image Credit: Wikimedia)
When is Corneal Topography Done?
Computerized corneal topography mapping can be helpful in the diagnosis of certain diseases and injuries of the cornea such as:
- corneal ulcer (central)
- corneal dystrophy
- bullous keratopathy
- progressing keratoconus
- astigmatism
Corneal topography is also beneficial in understanding post-traumatic corneal scarring disease, in LASIK during difficulty in fitting of contact lens, pre- and post penetrating keratoplasty, ocular surface disorder evaluation, refractive surgery screening and monitoring, etc.