What is DVT Prophylaxis?
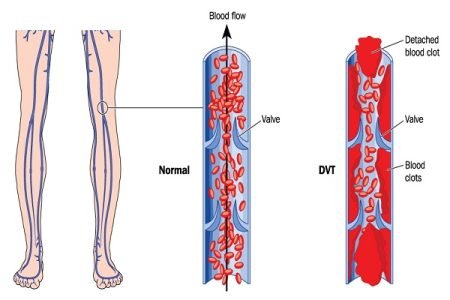
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are together known as venous thromboembolism (VTE). About 65% of the cases VTE manifest as DVT and rest as PE. Certain events can trigger venous thromboembolism and cause potentially life-threatening complications. One of the complications of VTE is trauma which is quite common in VTE patients and occurs in about 5 to 60% cases. There are several ways of managing DVT complications. One of them is DVT prophylaxis, which is necessary in the management of trauma patients particularly.
Thrombo-prophylaxis is considered to be an important patient safety procedure particularly in those patients who are admitted to the hospital after trauma or for a lower extremity surgery. Pulmonary embolism is the leading cause of in-hospital death that can be prevented. The risk of venous thrombosis in patients admitted to the hospital depends on various factors such as whether the admission is for medical or surgical purpose and also depends on the type of surgery.
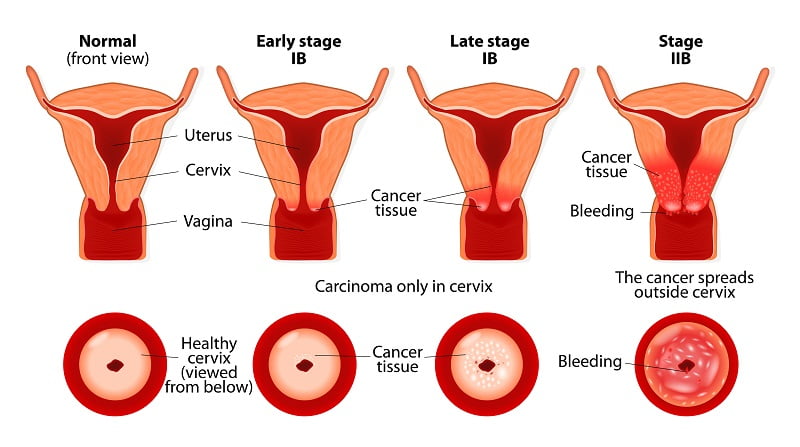
Venous thromboembolism (VTE) prophylaxis includes both pharmacologic and nonpharmacologic steps to reduce the risk of deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT of the leg occurs when there is a blood clot in the major veins in the leg or thigh, which impairs venous blood flow. This usually causes swelling and pain in the leg. PE occurs as a result of thrombus formation in distal veins, such as veins of the lower extremities.
How is DVT prophylaxis (deep vein thrombosis prophylaxis) therapy delivered?
The risk of developing VTE depends on a patient’s risk factors and the condition for which the patient is admitted to a hospital. VTE/PE prophylaxis can be done effectively through proper assessment of the various risk factors and medical conditions of the patient and by delivering an appropriate drug therapy and/or non-drug therapy to the patient accordingly.
When and how should you administer prophylaxis to prevent potential complications as a result of deep vein thrombosis (DVT) particularly after lower extremity surgery? Deep venous thrombosis (DVT) is though a rare but extremely devastating complication of foot and ankle surgery. It is more common in trauma patients. While many DVTs may remain subclinical or asymptomatic, DVT is a risk factor for a fatal condition called pulmonary embolism.
In order to manage the risks and benefits of DVT prophylaxis in patients who undergo lower extremity surgery, surgeons and healthcare providers must know the pathophysiology of deep vein thrombosis (DVT), the risks of associated with DVT for the proposed surgery, the risk of complications due to anticoagulation and various options available for prophylaxis. While DVT may develop in any deep vein, but it is more commonly seen in the veins of the lower extremity and pelvic region.
Traditionally, pelvic and lower extremity fractures, head injury, and immobilization have been considered as risk factors for VTE, however it is unclear which combination of risk factors defines a high-risk group for developing VTE. Options available for trauma patient thromboprophylaxis are of a variety of types – pharmacologic anticoagulation, mechanical prophylaxis, and inferior vena cava filters. The available pharmacologic agents include such as low-dose heparin, low molecular weight heparin, and factor Xa inhibitors. Mechanical prophylaxis methods include such as compression stockings, pneumatic compression devices, A-V foot pumps etc.
Guidelines recommend primary use of low molecular weight heparins in trauma patients, however there are still different views regarding the conclusive VTE prophylaxis in trauma patients. As of now, the optimal VTE prophylaxis strategy for trauma patients is not completely clear and known.
Options for VTE/DVT Prophylaxis
There are various options for DVT prophylaxis as discussed above. These may include both mechanical and pharmaceutical methods. The easiest method of prophylaxis is active range of motion of the ankles and the toes (lower extremity). This allows the muscles of the leg to function as a musculovenous pump to minimize stasis within the deep veins of the lower extremity. Sequential compression devices also help in prophylaxis as they serve to mimic the action of the muscles to stimulate blood flow through the vessels of the leg.
Physicians also recommend take aspirin for the prevention of DVT after the surgery but its efficacy is under debate. Aspirin does not affect the coagulation cascade. Aspirin may also have some other side effects such as erosion of the gastric lining and exacerbation of asthma in some patients.
Heparins work by affecting the coagulation cascade. Heparins inhibit the action of thrombin and other clotting factors by binding to antithrombin III. It is available as both subcutaneous and IV administrations. While heparins can reduce the occurrence of DVT and PE, they do have certain disadvantages.
Warfarin therapy is another form of prophylaxis, which is recommended by physicians frequently. Warfarin is a vitamin K analogue which inhibits the production of the vitamin K dependent factors as well as protein C and protein S.