Dermatologic Manifestations of Infective Endocarditis
- Updated on: Aug 3, 2024
- 4 min Read
- Published on Nov 11, 2019
Infective Endocarditis (IE)
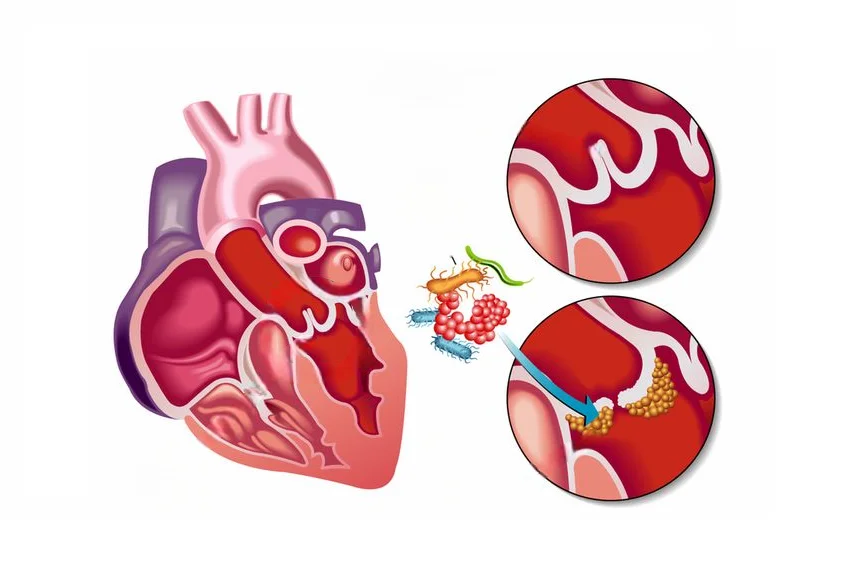
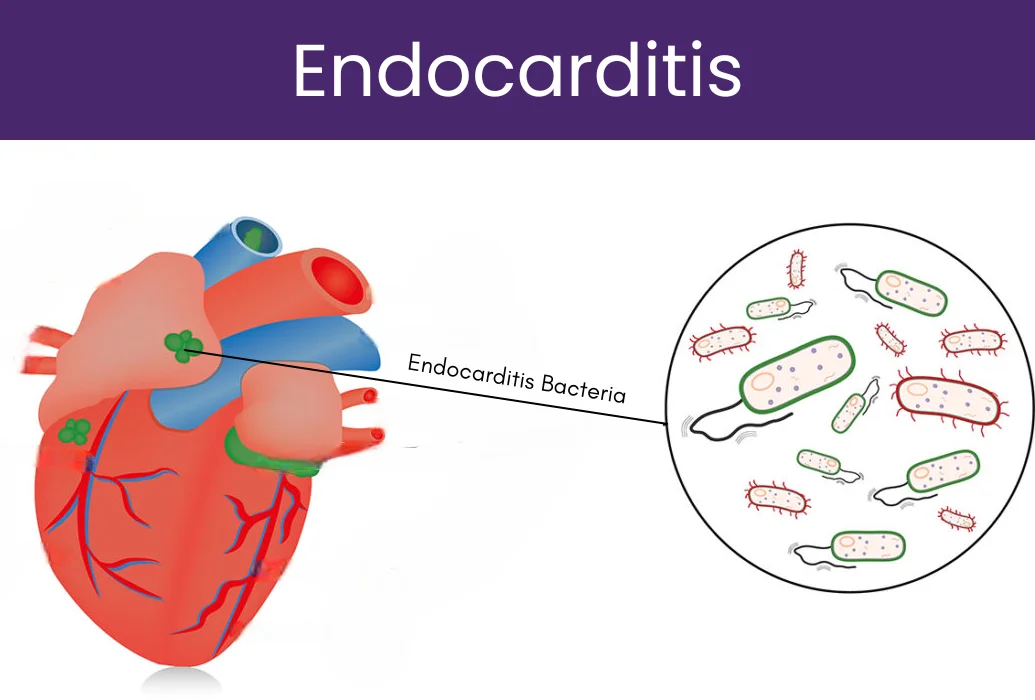
Infective endocarditis (IE) is the inflammation of heart valves and endocardial wall due to various infections. There are several microorganisms like bacteria, fungi which cause infective endocarditis. Its diagnosis is commonly based on various clinical, microbiological, and echocardiographic findings of the heart. Patients suffering from IE are given antibiotics according to the isolated causative microorganism.
Commonly, the highest rates of infective endocarditis are found in patients with prosthetic heart valves, intracardiac devices, unrepaired cyanotic congenital heart disease, previous history of IE, and intravenous drug use. However, there are almost 50 percent of IE patients who don’t have any previous history of valvular heart diseases.
It has been found that dermatological manifestations of IE have a very important role in the diagnosis of the disease. Moreover, dermatologic examination of patients with IE plays a crucial role in the evaluation of such patients.
Skin Changes Associated With Infective Endocarditis
Dermatological manifestations have a very important role to play in the diagnosis of infective endocarditis. Various skin related changes are found in IE patients, such as:
- Loss of color in skin
- Pale skin
- Appearance of new rash on skin commonly called as endocarditis rash
- Appearance of small red or dark spots under the skin on the toes, soles of the hands or feet, and fingers. These spots can either be painful or painless.
- Presence of small and tiny spots under the fingernails, on the chest, on the whites of the eyes, roof of the mouth, and on the inner side of cheeks.
Some Specific Dermatological Manifestations of Infective Endocarditis: Osler’s Nodes and Janeway Lesions
Despite advanced diagnostic and treatment options available for infective endocarditis, it still has a large number of morbidity and mortality rates. However, various dermatological examinations in IE suspected patients have been proven to be very useful. Various dermatological examinations in IE patients have revealed certain suggestive abnormalities of this disease like Osler’s nodes and Janeway lesions. Osler’s nodes are some purple colored lesions commonly found on the tips of fingers and toes in IE patients. These lesions are very painful. Janeway lesions are erythematous macules that usually affect palms of hands and soles of feet. They are generally painless.
Dermatologic examinations have been found to be very important diagnostic methods in the presumptive diagnosis of infective endocarditis. Among all of the IE dermatologic manifestations, Osler’s nodes and Janeway lesions are the most important ones. It has been found that Osler’s nodes are associated with sub acute IE while Janeway lesions are found in the acute forms of infective endocarditis. Therefore, the pathogenesis of both these dermatological findings remains controversial.
Osler’s nodes are painful lesions which usually last for few hours to several days. They are found on the thenar and hypothenar eminences (muscles present on the palm and at the base of the thumb) and the lateral side of the fingers. These lesions do not leave any sequelae. On the contrary, Janeway lesions last up to a few days or weeks. They are not painful and are commonly found on palms and fingers of hands, and soles of the feet.
The histological findings of both Osler’s nodes and Janeway lesions show presence of septic micro-emboli with dermal micro abscess formation. In addition, leukocytoclastic vasculitis has also been found. The culture tests may ultimately show a growth of the etiological agent of the infective endocarditis microorganism. Both Osler’s nodes and Janeway lesions are manifestations of IE with the only difference that Osler’s nodes are painful while Janeway lesions are painless macular lesions.
In addition to Osler’s nodes and Janeway lesions, cutaneous purpura is another most common skin manifestation of IE, but it is often misdiagnosed as a vasculitic rash of other etiologies. The differential diagnosis for a purpura patient must include a workup for endocarditis, particularly in patients with a known history of valvular disease or any other cardiac abnormality.
Some other cutaneous manifestations of IE are splinter hemorrhages under the nails, central nervous system effects like painful renal emboli, rarely gross hematuria, splenic emboli. Persistent infections may also result in splenomegaly or clubbing of the fingers and toes.
Prognostic Value of Dermatological Manifestations of Infective Endocarditis
Infective endocarditis (IE) being a rare disease has a very poor prognosis. A skin examination is important to look for a portal of entry and classic skin lesions to help diagnose and manage the condition. According to a research published in JAMA Dermatology journal in the year 2014, it has been found that among 497 definite infective endocarditis cases, 487 had known dermatological status, 11.9 percent had skin manifestations involving 8.0 percent with purpura, 2.7 percent with Osler nodes, 1.6 percent with Janeway lesions, and 0.6 percent with conjunctival hemorrhages (5 patients had 2 skin manifestations).
In addition, patients with skin manifestations had a higher rate of infective endocarditis-related extracardiac complications than patients without any skin manifestation. Also, purpura patients had larger cardiac vegetations. Infective endocarditis (IE) affects approximately 2 to 6 individuals per 100, 000 person-years in industrialized countries. A complete dermatological physical examination can be helpful for the management of IE in such cases.
Classic dermatological manifestations of IE are signs of infection severity and help physicians to look for secondary complications. In addition, dermatological manifestations also have a prognostic role in infective endocarditis and influence therapeutic decisions.