Diabetic Neuropathy and Nerve Damage
- Updated on: Jan 20, 2024
- 6 min Read
- Published on Sep 4, 2022
What is Diabetic Neuropathy?
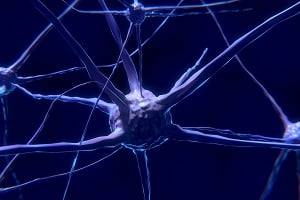
Diabetic neuropathy is a type of nerve damage that is caused by diabetes. It is a complication of diabetes. High blood sugar (glucose) in diabetic patients can damage your nerves throughout the body. Diabetic neuropathy mostly affects the nerves in your feet and legs.
Different types of nerve damage can result in different symptoms which can range from problems like pain and numbness in your feet to functioning of your internal organs like your heart, bladder, and digestive system. Diabetic neuropathy symptoms vary in different people. Some people may present mild symptoms while others may present symptoms that are very painful and disabling.
How Does Diabetic Neuropathy Occur?
Even though there is no exact cause of diabetic neuropathy but some researchers in the medical community suggest that the inability to control normal blood glucose levels can be a major factor for the development of diabetes-related nerve damage or simply diabetic neuropathy. However, the exact mechanism behind diabetic neuropathy due to high blood glucose levels is still unclear. Learn about blood glucose charts that you will need if you have diabetes.
Prolonged exposure to high blood glucose levels is believed to be responsible for the destruction of blood vessels. Such damaged blood vessels become unable to supply essential nutrients and oxygen to the nerves and ultimately destroy the nerves leading to nerve damage or diabetic neuropathy.
Following factors have been somehow found to be responsible for diabetic neuropathy:
LifeStyle
Excessive consumption of alcohol and smoking can lead to diabetic neuropathy.
Age
Older people who are suffering from chronic diabetes are believed to be more prone to diabetic neuropathy.
Nerve Injury
Any injury to nerves whether due to inflammation or any other cause can make them susceptible to diabetic neuropathy.
Autoimmune Factors
Autoimmune diseases like diabetes type 1 can turn the immune system against its own body resulting in inflammation and ultimately nerve damage.
Genetic Factors
Some people can inherit a gene responsible for diabetic neuropathy and due to which they may be more susceptible to nerve damage.
Metabolic Factors
Besides high blood glucose and chronic diabetes, excess levels of fats in the blood are responsible for diabetic neuropathy.
Progression of Diabetic Neuropathy
The nerve damage caused by diabetes often gets worse over time, especially in people with chronic diabetes. The nerve damage starts slowly and sometimes gets unnoticed. As the disease progresses, diabetic neuropathy symptoms start appearing and then affect your normal life. It is suggested that almost 7 out of 10 diabetes people develop diabetic neuropathy. Progression of diabetes to diabetic neuropathy is common in people who:
- Are overweight
- Have/had diabetes for more than 25 years
- Are unable to control their blood sugar
- Are suffer with hypertension (hypertensive people)
- Have hyperlipidemia
- Are smokers
The exact cause behind diabetic neuropathy progression is still unknown. There’s not a single cause and the causes can vary among different people. However, prolonged high blood sugar levels seem to be one of the major causes. High blood sugar damages nerve cells and blood vessels directly through chemical changes or inflammation.
When blood vessels that supply nerves get damaged, the progression of the disease occurs. Initially, only the outer lining of nerves gets affected due to nerve damage but with time, actual nerve fibers are damaged which ultimately results in the loss of nerve fibers. The effect of the progression of nerve damage depends on the types of nerves affected.
The progression of diabetic neuropathy can occur almost anywhere in the body. Some of the examples are:
Peripheral Diabetic Neuropathy Progression
This type of diabetic neuropathy occurs in the nerves present in the outer limbs like feet and hands. Symptoms usually begin in the feet and legs and may include pain, numbness, and tingling. As the neuropathy progresses, the following changes may occur in your outer limbs (feet and hands):
- Structural changes in the feet
- Frequent feet infections that may get worse and require amputation of a foot or leg
- Weakness
- Muscle shrinkage
- Difficulty in walking and maintaining balance
- Autonomic Diabetic Neuropathy Progression
Autonomic Neuropathy Progression
This type of nerve damage affects the nerves responsible for controlling your body’s automatic functions. Such nerves include those nerves that control your heart, bladder, digestion, and sexual functions. Initially, there are no symptoms in this type of diabetic neuropathy but as the disease progresses following symptoms may appear:
- Changes in sweating
- Dizziness especially when you stand up
- Nausea and fullness after eating
- Loss of appetite
- Sexual problems in both men and women
- Bladder problems
- Vision problems at night
How Can We Detect the Early Progression of Diabetes Towards Nerve Damage?
Early detection of diabetes progression towards nerve damage can be very helpful in preventing nerve damage and associated complications. This can be done by taking a few simple measures like:
- Attending regular screening for diabetes type 2 after the age of 45 or before
- Maintaining normal glucose levels in the blood especially if you are diabetic (glucose levels of 126 mg/dl or higher indicate diabetes)
Diabetics present different symptoms that can signal the onset of diabetic neuropathy. People who have diabetic neuropathy will often experience the following symptoms and should consult the doctor immediately:
- Pain, soreness and stiffness
- Nausea
- Vomiting
- Impaired sense of hunger, which may lead to overeating
- Joint damage, especially in the feet and legs
- Excessive or decreased sweating
- Muscular problems like muscle wasting
- Frequent skin infections that take longer time to heal, particularly on the feet
In all the above-mentioned cases, controlling blood sugar levels is the only way to prevent the disease from becoming worse. Patients with high blood glucose levels but not that much high which will lead to diabetes are called prediabetics. Prediabetics have blood glucose levels of almost 100–125 mg/dl. It can be reversed by making some lifestyle changes in terms of diet and physical exercise.
We Should Stay Ahead of Diabetic Neuropathy
We can stay ahead of diabetic neuropathy and prevent the associated nerve damage by following some healthful tips:
Foot Examination
A comprehensive foot examination is a good way to check peripheral neuropathy in diabetics. Regular foot checkups are very useful to catch nerve damage and other related problems early. While having a foot examination, you should always share your symptoms with your doctor like pain, numbness, tingling, and loss of sensation in your feet.
Control Blood Sugar
Maintaining normal blood sugar levels can slow the development of diabetic neuropathy.
Follow a Heart-Healthy Lifestyle
Following a heart-healthy lifestyle can help in preventing diabetic neuropathy. Some studies suggest it to be very helpful in preventing the risks caused due to the autonomic nerve damage of the heart in people with type 1 and type 2 diabetes.
Why is it Important to Take Care of Your Feet in Diabetic Neuropathy?
Peripheral neuropathy is a type of neuropathy that mostly occurs in the lower limbs like feet. People suffering from diabetic peripheral neuropathy often start losing their sense of feeling in their feet. As a result, they are more likely to hurt themselves, walk abnormally, and even develop feet sores that are difficult to heal. Feet sores caused by diabetic nephropathy get worse over time and can lead to amputation of your feet or legs. For avoiding these serious complications diabetic people need to keep a close eye on their feet and maintain proper foot care.
Diabetics, who already have signs of nerve damage, should get their feet examined regularly. This will help them in noticing as well as treating feet related issues before they cause more harm.
Following are some ways in which you can care for your feet while living with chronic diabetes:
- Examine your feet and legs regularly for any cuts or sores
- Regular nail care
- Use comfortable and properly fitting shoes to avoid foot sores
- Apply lotion if you have dry feet (but not between the toes)
- Avoid extreme hot water for bathing
What is Neuropathic Arthropathy Progression or Charcot Joint?
Diabetic nerve damage can sometimes lead to joint damage called ‘Neuropathic Arthropathy’. This mostly occurs in the foot and ankle joints. The condition often presents symptoms of numbness and loss of feeling in your foot and may present the following other symptoms in the advanced stage:
- You become unaware of the stress on your foot and ankle
- Your ankle and foot joints may need support due to loss of muscle strength
- You could hurt, twist, or damage your foot or ankle and not know it due to loss of sensation
- Your foot and ankle joints may start to grate on each other
- Your joints may be collapsed
- Your joints become deformed
The best way to prevent diabetic neuropathy from progressing is to control your blood sugar levels by coordinating with your doctor about various diabetes management techniques. You should also reduce your risk factors by maintaining a healthy lifestyle.
FAQs
How does diabetes contribute to nerve damage and neuropathy?
Elevated blood sugar levels over time can lead to nerve damage by affecting blood flow and causing inflammation, resulting in diabetic neuropathy.
Are all diabetics at risk of developing diabetic neuropathy?
While not inevitable, all diabetics are at risk. Consistent blood sugar management and healthy lifestyle choices can significantly reduce the risk of developing diabetic neuropathy.
What are the early signs of diabetic neuropathy that one should be aware of?
Symptoms may include tingling, numbness, or pain in the extremities. Regular check-ups and prompt reporting of any unusual sensations are crucial for early detection and intervention.
Can diabetic neuropathy be reversed or only managed?
Early intervention and optimal blood sugar control can sometimes slow or halt the progression, but complete reversal is challenging. Management focuses on symptom relief and preventing further damage.
How often should individuals with diabetes undergo screenings for neuropathy?
Annual screenings, or more frequently as advised by healthcare providers, are recommended to detect early signs of neuropathy and initiate timely interventions.