Endometrial Cancer: Causes, Symptoms, Diagnosis, Treatment, Risks, Prevention
- Updated on: Jul 8, 2024
- 15 min Read
- Published on Sep 27, 2019
Overview and definition of endometrial cancer: What is endometrial cancer?
Endometrial cancer is a type of cancer that develops in the cells of the inner lining of the uterus (called endometrium). The cells in endometrium begin to grow in an uncontrolled manner. Endometrial cancer is sometimes called uterine cancer also. Other types of cancer can also develop in the uterus such as uterine sarcoma. But, these cancers are not as common as endometrial cancer.
Facts and important information about endometrial cancer
- Endometrial cancer or endometrial neoplasm (malignant neoplasm of endometrium) is a cancer in which malignant cells develop in the tissues of endometrium in women.
- Common signs of endometrial cancer are vaginal bleeding or pelvic pain.
- Diagnosis of the endometrium aims to detect the cells in the lining of the uterus that might be cancerous. Pap tests don’t always detect the endometrial cancer, and most women who get it have normal findings.
- Obesity, having diabetes, and metabolic problems can increase the risk of endometrial cancer.
- Tamoxifen that is used for breast cancer can increase the risk.
- Going through menopause later than normal or having your first period at an extra young age can also increase the risk.
- Use of estrogen hormones alone can also increase the risk of endometrial cancer.
- One can develop endometrial cancer in any age, but it’s most common when you are 45-74 years old.
- The most important thing you can do to avoid endometrial cancer is to know the early warning signs.
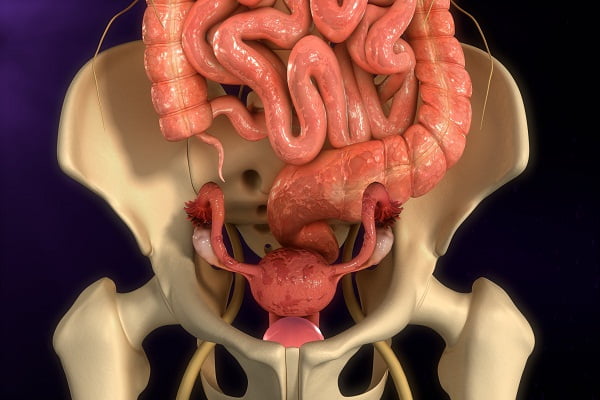
What are uterus and endometrium?
The uterus is a hollow and muscular organ where a fetus grows and develops when a woman is pregnant. It is located in the pelvic region. It is normally about the size and shape of a medium-sized pear. A woman’s uterus has 2 main parts:
- Cervix: It is the lower end of the uterus that extends into the vagina
- Corpus: It is the upper part of the uterus and is also called the body of the uterus
Endometrium is the lining of the uterus. Cancer of the endometrium is different from the cancer of the muscle of the uterus (body of the uterus), which is called sarcoma of the uterus.
Types of cancers of the endometrium
Endometrial carcinomas or endometrial cancers can be classified into various types based on how the cells appear under a microscope view. These are such as:
- Adenocarcinoma: Most cases of endometrial cancers are adenocarcinomas
- Carcinosarcoma
- Small cell carcinoma
- Transitional carcinoma
- Squamous cell carcinoma
- Undifferentiated carcinoma
The most common of all adenocarcinoma is endometrioid cancer. There are many sub-types of endometrioid cancers, such as:
- Adenocarcinoma
- Ciliated carcinoma
- Villoglandular adenocarcinoma
- Adenoacanthoma
- Adenosquamous
- Secretory carcinoma
Causes of endometrial cancer: What causes endometrial cancer?
We do not know much about what exactly causes endometrial cancer. A lot of research is in progress to understand more about the disease.
Most cases of endometrial cancer cells contain estrogen and/or progesterone receptors on their surfaces. Therefore, scientists believe that interactions of these receptors with their hormones might be responsible for an uncontrolled growth of the endometrium cells leading to endometrial cancer.
The most common cause of endometrial cancer is too much of the hormone estrogen compared to the hormone progesterone in the body. This causes an imbalance in the hormones, which eventually causes the lining of the uterus to get thicker. If this continues, the cancer cells can grow out of control.
Women who have this hormone imbalance over time are more likely to develop endometrial cancer in later ages such as after they are 50 years.
Risk factors for endometrial cancer
It is important to know that having a risk factor for a disease does not mean that you will get it. If you are at an increased risk for endometrial cancer, it does not mean you will necessarily get it. Similarly, not having risk factors doesn’t always mean that you will not get cancer. You must talk to your doctor if you think you may be at risk for endometrial cancer.
Some women with endometrial cancer do not have any known risk factors. Even if a woman has one or more risk factors, it is not possible to know exactly which of these factors might be responsible for the cancer.
Although the exact cause of endometrial cancers is unknown, there are certain risk factors that may increase the women to develop in. These may include such as women with endometrial overgrowth (hyperplasia), women who have never had children, obesity, menstruation at an early age, delay in menopause, estrogen therapy, using tamoxifen alone, radiation therapy for the pelvis, family history, Lynch syndrome (which is an inherited form of colorectal cancer).
Common and important risk factors are described herein:
Hormone factors
As mentioned above, hormone imbalances may disturb the normal growth of cells and might play a part in the development of endometrial cancers. In fact, most endometrial cancers occur due to a disturbance in their hormone balance. Many known risk factors for endometrial cancer cause a change in their estrogen levels.
Before a woman has menopause, ovaries produce two main types of female hormones called estrogen and progesterone. The balance between these two hormones changes during a woman’s menstrual cycle each month. This keeps the endometrium of a woman healthy. A change in this balance of estrogen and progesterone (in which a shift occurs toward producing more estrogen) increases the risk of getting endometrial cancer.
After a woman has menopause, her ovaries stop making these hormones. However, her body still produces a small amount of estrogen in fat tissues. Estrogen from fat tissues has a bigger influence after menopause than before menopause.
Estrogen therapy
Menopausal hormone therapy also sometimes called hormone replacement therapy is also responsible to increase the risk of endometrial cancer. Estrogen is primarily used in this therapy, which can also cause an imbalance between the two hormones. Use of estrogen alone (without any progesterone) can cause type I endometrial cancer in women. In order to reduce this risk, progestin progesterone must be given along with estrogen in the therapy. This is called combination hormone therapy.
Women who do not take progesterone along to treat menopausal symptoms do not have an increased risk of endometrial cancer. But, doctors have found that taking this combination also increases a woman’s chance of developing other cancers such as breast cancer and also increases the risk of other diseases.
There is enough epidemiologic evidence that postmenopausal estrogen therapy substantially increases the risk for endometrial cancer. According to a research, since 1970, more than 30 epidemiologic studies have documented the strong association between unopposed estrogen use and increased endometrial cancer risk. The risk is increased with an increase in the dosage of estrogen and duration of use. Women who use it for more than 10 years continuously have a 10-times increased risk of developing this cancer.
Menstrual cycles
The risk of endometrial cancer increases with having more menstrual cycles during lifetime. Starting menstrual periods at an early age (before age 12) and/or going through menopause later in life also increases the risk of endometrial cancer.
Birth control pills
Birth control pills such as oral contraceptives can reduce the risk of endometrial cancer. The risk is lowest in women who take the pill for a long time. The risk remains lower even several years after a woman stops taking these pills.
The more periods you’ve, the more exposure your endometrium has to estrogen.
Pregnancy
Women who have never been pregnant are at higher risk of endometrial cancer than those women who have had at least one pregnancy. This is because the hormonal balance shifts toward more progesterone during pregnancy. Therefore, having several pregnancies protects women against endometrial cancer.
Women who have had no pregnancy, especially if they were infertile (unable to become pregnant) also are even at higher risk of this cancer.
Tamoxifen
Tamoxifen is a drug used to prevent and treat breast cancer. It works as an anti-estrogen in breast tissue, but it acts as an estrogen in the uterus. The drug can cause the uterine lining to grow in some women, which can increase their risk of developing endometrial cancer. However, the risk of developing endometrial cancer from tamoxifen is low.
Your doctor will evaluate whether the harms with taking tamoxifen balances against the benefits of this drug in treating and preventing breast cancer. If you are taking tamoxifen, your doctor may recommend for regular tests and exams to make sure that any sign of endometrial cancer can be reported early on.
Ovarian tumors
Certain types of ovarian tumors make estrogen. Estrogen release by these tumors may not be controlled and can sometimes lead to higher levels of the estrogen. This may result in a hormonal imbalance and lead to endometrial cancer. Vaginal bleeding is a common sign of endometrial cancer in such tumors.
Obesity
Ovaries produce most of the estrogen in a woman’s body, but fat tissue can also convert some other hormones into estrogens. Fat tissue can increase a woman’s estrogen levels, which eventually increases the risk of endometrial cancer. Women who are obese are thrice at risk for endometrial cancer as compared to women who maintain a healthy weight.
Polycystic ovarian syndrome
Polycystic ovarian syndrome (PCOS) can cause abnormal hormone levels in women. The increase in estrogen compared to progesterone in women due to PCOS can put a woman at higher risk of getting endometrial cancer.
Intrauterine devices
Scientists believe that women who use an intrauterine device (IUD) for birth control are likely to be at lower risk of developing cancer of the endometrium.
Age
The risk of endometrial cancer increases with age.
Diet and exercise
A high-fat diet can increase the risk of cancers, including endometrial cancer. Fatty foods are high-calorie foods, which leads to obesity. Obesity is a commonly understood risk for endometrial cancer. Some researchers believe that fatty foods may have a direct influence on your estrogen levels, which is a major endometrial cancer risk factor.
Inherited colon cancer syndrome
Hereditary nonpolyposis colorectal cancer (HNPCC) increases the risk of colon cancer and other types of cancers, including endometrial cancer. HNPCC is caused by a gene mutation that is passed off from parents to children.
Other risk factors for endometrial cancer
- Having metabolic syndrome
- Having type 2 diabetes
- Exposure of endometrial tissue to estrogen made by the body for various reasons
- Having certain genetic conditions such as Lynch syndrome
- Having endometrial hyperplasia
- Having been diagnosed with breast cancer or ovarian cancer in the past
- Treatment with radiation therapy to the pelvis
Prevention of endometrial cancer
Cancer prevention is thee action taken to lower the chances of developing cancer. Prevention measures can help reduce the number of new cases of cancer within a population group. This eventually lowers the number of deaths caused by the cancer every year.
Can Endometrial Cancer Be Prevented?
In most cases, the endometrial cancer cannot be prevented. However, there are ways to lower the risk of developing or spreading the cancer.
Scientists try to identify the risk factors to prevent the cancer from developing or spreading. Some risk factors can be avoided, but others cannot. Different risk factors contribute to different types of cancer. Research is being done to identify different ways of preventing endometrial and other types of cancers. Scientists are investigating what factors can increase your risk for this type of cancer.
Although there is no known way till date to completely prevent endometrial cancer, you may be able to reduce the risk by following these guidelines. Talk to your doctor for more information about your individual risk of endometrial cancer.
What are the ways to lower the risks and prevent endometrial cancer?
Get proper treatment for your endometrial problems
It is important to get proper treatment of pre-cancerous disorders of the endometrium. Most cases of endometrial cancers occur gradually over a period of several years. Many of them are easy to detect at an early pre-cancerous stage and usually start from less serious problems of the endometrium. One of the abnormalities that may contribute to the development of endometrial cancer is hyperplasia. Though the disease go away without treatment after some time, but it can sometime require more careful attention and treatment with hormone therapies or surgery such as hysterectomy. This can prevent the disease to become cancerous. Abnormal vaginal bleeding is a common symptom of endometrial pre-cancers and cancers, and it requires prompt evaluation and treatment.
Common symptoms of hyperplasia are heavy menstrual periods, bleeding between the periods, and bleeding after menopause.
Evaluate benefits and dangers of hormone therapy
Hormone therapies of estrogen are generally recommended to treat the symptoms of menopause through different forms such as pills, shots, creams, etc. You must ask your doctor about your risk of developing endometrial cancer as a result of the hormone therapy.
Progestins or drugs similar to it can help reduce the risk of endometrial cancer in women who take estrogen therapy. However, this combination therapy increases the risk of breast cancer, as found in some studies. Particularly, if you had not gone through hysterectomy and still have the uterus and are going through hormone (estrogen alone) therapy, you must evaluate the risks of developing various types of cancers with your doctor.
Exercises
Research shows that exercises and higher levels of physical activity lower your risk of getting endometrial cancer. It is to good engage in regular physical activity (such as exercise) to possibly prevent endometrial cancer.
An active lifestyle can help maintain a healthy weight and avoid problems such as high blood pressure and diabetes, which are some other risk factors for endometrial cancer.
Get proper treatment of hereditary nonpolyposis colon cancer (HNPCC or Lynch syndrome)
As discussed above, women who have hereditary nonpolyposis colon cancer (such as HNPCC or Lynch syndrome) are at an increased risk of endometrial cancer.
One of the ways to lower their risk of getting endometrial cancer is to remove the uterus through a process called hysterectomy. However, women who want to have children in future may not want to choose it.
Avoiding other risk factors and adapting to protective factors can help prevent endometrial cancer
Avoiding cancer risk factors discussed above may help prevent it. Increasing protective factors such as quitting smoking and increasing physical activity levels may also help prevent the cancer.
Protective factors that decrease the risk of endometrial cancer and help prevent it
The following protective factors decrease the risk of endometrial cancer:
Pregnancy and breast-feeding
Estrogen levels are lower in pregnancy and when breastfeeding. The risk of endometrial cancer is reduced with children, particularly, at an early age (before 30 years). Breastfeeding at an early age in women for about 2 years also decreases the risk of endometrial cancer.
Breast-feeding decreases ovulation and estrogen activity.
Combination oral contraceptives
Contraceptives that contain both estrogen and progestin decrease the risk of developing endometrial cancer. The more duration for they are consumed, the more are the benefits. In fact, their effects can last for many years even after a woman stops using them.
However, these contraceptives do have certain side effects such as being at higher risk of blood clots, stroke, and heart attack, especially for women who are older than 35 years. Therefore, you should discuss the pros and cons of these oral contraceptives with your doctor before you plan to use them regularly.
Diet
A diet that is low in saturated fats and high in fruits and vegetables may lower the risk of endometrial cancer. The risk may also be lowered when soy -based foods are a regular part of your diet. In some studies, however, fruits and vegetables are found to have no direct influence on the risk of developing endometrial cancer in women.
Cigarette smoking
If you are smoking 20 cigarettes a day, you are at lower risk of endometrial cancer. The risk of endometrial cancer is even lower in women who smoke after menopause. However, there are many other dangers of smoking, which does not justify smoking as a prevention measure for endometrial cancer. These disease could be severe and life-threatening in the long run such as:
- Lung cancer
- Heart diseases
- Cancers of the head and neck
- Pancreatic cancer
- Bladder cancer
Others factors that are not proven yet to influence the risk of endometrial cancer
- Fruits, vegetables
- Weight loss
- Vitamins and multi-vitamins
REMEMBER: You have no risk for endometrial cancer if you have had your uterus removed (through a procedure called hysterectomy).
Clinical trials for cancer prevention are used to study how to prevent endometrial cancer (and other cancer types)
Cancer prevention clinical trials are used to find ways to reduce the risk of developing certain types of cancer such as endometrial cancer. Some cancer prevention trials are conducted with healthy people who have not had cancer but who are at an increased risk for the cancer. Other prevention trials are done with people who have had cancer and are trying to prevent another cancer of the same type or to lower the risk of developing a new type of cancer. Other trials are done with healthy volunteers who are not known to have any risk factors for any type of cancer.
The objective of some cancer prevention clinical trials is to find out whether actions people take can prevent cancer. These may include eating fruits and vegetables, exercising, quitting smoking, or taking certain medicines, vitamins, minerals, or food supplements.
New ways for the prevention of endometrial cancer are being investigated in clinical trials
Clinical trials are taking place in many parts of the world. Information about clinical trials can be found in the Clinical Trials section of the websites of respective countries. You can check out NCI’s list of cancer clinical trials for endometrial cancer prevention trials that are now accepting patients in the United States, for example. You can request for enrollment as a participant if you think you are a likely candidate and can benefit from it.
Early detection of endometrial cancer
Early detection of cancer means identifying for the cancer before a person has its symptoms. This can sometimes find the disease early, which can lead to early treatment. This improves the chance that treatment will work and the person’s life can be saved or improved.
Can Endometrial Cancer Be Found Early?
In most cases, identifying the signs and symptoms of endometrial cancer early and reporting them promptly to the doctor allows the cancer to be diagnosed at an early stage. Early detection of endometrial cancer improves the chances that the cancer will be treated early and successfully. However, not all cases of endometrial cancer can be detected early. Some types of endometrial cancers may progress to an advanced stage before any signs and symptoms are noticed by the patient.
If detected early and treated well on time, endometrial cancer provides a good prognosis. About 81 percent of women are likely to live five years after the diagnosis in such cases. Many of them can live much longer than this. But if the cancer returns and spreads after the treatment, it can be more dangerous.
What is endometrial cancer screening?
Screening for endometrial cancer is the method of looking for cancer before a person has any noticeable symptoms. This can help find the cancer at an early stage. When abnormal tissue or cancer is found early during screening tests, it may be easier to treat it better and on time. Otherwise, by the time symptoms appear, it’s already too late and cancer may have spread to other parts of the body.
Early detection allows the use of tests to find a disease such as cancer in people who do not have symptoms of that disease.
Scientists are trying to gather information that can help doctors recommend who should be screened for endometrial cancer and which screening tests, in particular cases, should be used and how often.
It is important to know that you may not necessarily have cancer if your doctor suggests a screening test for it. Screening tests are done when you have no cancer symptoms at all. They are considered a prevention strategy.
If a screening test result is abnormal, you may need to have more tests done to find out if you have the cancer. These are called diagnostic tests.
There is no single screening test for endometrial cancer that can completely detect the cancer. This means women should stay alert for the symptoms and follow the guideline of their doctors if they are at high risk of developing the cancer.
Tests for early detection or screening of endometrial cancer
Screening tests are procedures to prevent the disease. There are no routine tests used to screen for endometrial cancer, but if your doctor thinks you are at higher than average risk of endometrial cancer, he or she can check for it in the following ways:
Transvaginal ultrasound (TVU)
In this test, a probe is inserted into the vagina to generate images of the uterus. The probe sends out sound waves that echo off the walls of the uterus. These waves are translated into images. The inside of the uterus and changes in the thickness of the lining can be seen through this procedure. An ultrasound is generally used in the beginning to see if a biopsy is needed for ruling out other possibilities.
Pelvic ultrasound
A probe is moved over the skin of lower belly to get images of your uterus instead of in the vagina as done in transvaginal ultrasound. A gel is applied on the skin to slide the probe and get clear images. You may be asked for a full bladder before this test.
Endometrial sampling (Biopsy, Hysterescopy, Dilation and Curettage)
A sample of the cells is taken from the lining of the uterus. The procedure can be done in many ways. An endometrial biopsy is one of the methods. It uses a thin flexible tube that’s put through your vagina and cervix into the uterus. Cells are than removed through the tube.
A hysteroscopy is another procedure which allows your doctor see inside the uterus. It’s done with a small telescope kind of tool. The telescope is inserted into the vagina and the cervix. Tissues can be taken too. Polyps or other abnormal tissues can also be removed in this procedure. If the doctor determines to extract more cells, he or she may conduct a dilation and curettage (D&C) procedure.
In a dilation and curettage procedure, drugs may be introduced in the body to help you relax and sleep. A special tool is inserted through an opened (dilated) cervix. Your doctor will remove the lining of the uterus. Sampled of the cells may be taken which are investigated under a microscope for cancer.
Early detection (screening) according to different levels of risks for endometrial cancer
Women at an average risk for endometrial cancer
There are no screening tests or exams to find endometrial cancer early in case you are at an average endometrial cancer risk and experience no symptoms.
According to The American Cancer Society, at menopause, all women should be told about the risks and symptoms of endometrial cancer and strongly encouraged to report any vaginal bleeding, discharge, or spotting to their doctor.
Women should get regular pelvic exams, which can help detect some cancers. But these tests are not very effective in finding early endometrial cancers.
Pap test is a well known test to screen women for cervical cancer. It can occasionally find some early endometrial cancers, but it’s not a very good test for this type of cancer.
Women at increased endometrial cancer risk
According to The American Cancer Society, women who are at an increased risk of endometrial cancer should be informed of the risk and be asked to see their doctor whenever they notice any symptoms such as vaginal bleeding, abnormal discharge etc.
Women’s risk of endometrial cancer may be increased due to increasing age, late menopause, never had child birth, infertility, obesity, diabetes, high blood pressure (hypertension), estrogen therapy, or tamoxifen therapy etc.
Who may need screening for endometrial cancer?
Doctors recommend screening tests for the cancer if you are at more than average risk for cancer. Your healthcare provider may advise screening in these situations:
- You may have genes with hereditary nonpolyposis colon cancer (HNPCC). Your doctor may ask if HNPCC runs in your family. You may have this gene if other types of cancer such as colon cancer, ovarian cancer, or uterine cancers run in your family.
- You have known risk factors and are going through menopause stage.
- You have pre-cancerous changes (such as hyperplasia) in the cells inside your uterus. These cells may turn into cancer.
According to The American Cancer Society, women who have or may have HNPCC must be offered yearly testing for endometrial cancer with endometrial biopsy beginning at age 35. Doctors should discuss this test, its risks, benefits, limitations with them. This is applicable for women who are known to carry HNPCC-linked gene mutations, women who are likely to carry such a mutation (those with a mutation known to be present in the family), and women from families with a tendency to get colon cancer where genetic testing has not been done.
A woman who have (or may have) HNPCC may be asked for a hysterectomy if she is not planning any children in future.
More research funding needed for endometrial cancer
The main treatment for endometrial cancer is a hysterectomy. It involves surgically removing the uterus of a woman. The fallopian tubes, ovaries, and some lymph nodes may also be taken out at the same time depending on the risk of spread of cancerous cells to the nearby areas.
A hysterectomy can be done through minimally invasive routes too. The uterus also can be taken out either robotically or laparoscopically in minimally invasive approaches.
Sometimes, further treatment may be needed such as radiation, hormonal, or chemotherapy etc.
There is a need for more funding of research and clinical trials to help provide better treatment for women whose endometrial cancer has returned.
Endometrial cancer’s mortality is increasing and the funding for it is relatively very low. There is a need for more research on this cancer and more clinical trials to fight this disease.
Signs and Symptoms of Endometrial Cancer
There are a few symptoms that may indicate the chances of endometrial cancer. Some of them are more common when the cancer is at a later stage.
Unusual heavy vaginal bleeding, spotting, or other abnormal discharge from vagina
Most women diagnosed with endometrial cancer experience abnormal vaginal bleeding. These may include changes in their menses or bleeding between periods or after menopause.
Such types of discharge or vaginal bleeding can occur in some non-cancerous












