Esophageal Cancer: Causes, Signs, Symptoms, Diagnosis, Treatment, Stages, Surgery, Prevention, Survival
- Updated on: Jul 10, 2024
- 24 min Read
- Published on Sep 27, 2019
What is esophageal cancer – Definition and overview?
Esophageal cancer is described as the disease of esophagus where the cells lining the esophagus mutate or change and become cancerous (malignant). Uncontrolled growths of these cells form a mass or tumour in the esophagus (oesophagus) which may spread to other parts of your body. Sometimes, many other names are used for it such as cancer of the esophagus, cancer of the gullet and cancer of the food pipe etc.
Oesophageal cancer is ranked as sixth most common cause of cancer deaths worldwide. However, different geographic locations have different Incidence rates. The cause of higher incidence rates of esophageal cancer cases in some regions may be attributed to higher tobacco and alcohol use or particular nutritional habits and obesity in the region.
Failed early diagnosis and treatment of oesophageal cancer can result in its spreading through the lymphatic system to nearby lymph nodes or through the bloodstream to other parts of the body, most commonly the liver. It can also invade the windpipe and lungs by growing through the esophagus wall.
Anatomy and physiology of the esophagus
To better understand esophageal cancer, one must know the normal structure and function of the esophagus.
The esophagus is a part of upper gastrointestinal tract (GI Tract) which is a sub-section of your digestive system and lies behind the wind pipe or trachea and in front of the spine. It is a long and hollow muscular tube measuring about 20-25 cm in length and 2-3 cm wide that serves as a passage for moving food and drink from the mouth to the stomach.
The upper part of the esophagus at its beginning is guarded by a special ring of muscle that relaxes and opens the esophagus when the food or liquid comes toward it and is called the upper esophageal sphincter.
The point where the esophagus connects with the stomach is called the gastroesophageal (GE) junction. The lower esophageal sphincter – a special ring of muscle near the GE junction is responsible for controlling the movement of food from the esophagus into the stomach. When you are not having meals, this sphincter remains closed to keep the stomach’s acid and digestive juices out of the esophagus.
The wall of the esophagus is composed of several layers of the tissues. Esophageal cancer usually starts and grows in these layers. For this reason, it is important to have an understanding of these layers of the esophagus wall.
Layers of the esophagus wall
The different layers of the tissues present in esophagus wall include:
- Mucosa – this is the most innermost layer and is made up of squamous cells
- Submucosa – this is the supporting layer of the mucosa and have glands which produce mucus and also contain blood vessels and nerves
- Muscle layer – this is also known as muscularis propria and is responsible for contraction and relaxation of esophagus which helps in the movement of food through it
- Outer layer – also called as adventia and consists of connective tissues which support the esophagus
How common is oesophageal cancer? Who gets oesophageal cancer?
According to the American Cancer Society’s estimation of esophageal cancer in the United States for 2018:
- About 17,290 new oesophageal cancer cases will be diagnosed which will include 13,480 men and 3,810 women
- Deaths from esophageal cancer will be about 15,850 which includes 12,850 men and 3,000 women
About 1% of all cancers diagnosed in the United States belong to the esophageal cancer category, and other parts of the world where it is more common includes Iran, northern China, India, and southern Africa.
Men are three times more likely to develop oesophageal cancer than women. The lifetime risk of esophageal cancer in the United States for men is about 1 in 132 while it is about 1 in 455 for women. It is more common among people of age group 60-70 years but can occur at any age.
What are the different types of esophageal cancer?
The type of oesophageal cancer signifies the type of cell that the cancer started in. The oesophageal cancer usually starts in the mucosa (inner layer) and grows outward through the submucosa and the muscle layer. Since esophagus wall is lined by 2 types of cells, there are 2 main types of oesophageal cancer.
- Squamous cell carcinoma
- Adenocarcinoma
Squamous cell carcinoma
Squamous cells make the innermost layer of the esophagus and are responsible for its lining. Cancer starting out of these cells is called squamous cell carcinoma.
The occurrence of squamous cell carcinoma can happen anywhere along the length of esophagus, but the esophagus located in the neck region and in the upper two-thirds of the chest cavity are the major locations where they are found. This type of cancer used to be responsible for the majority of esophageal cancer cases in the United States earlier, but with time it has changed and now it accounts for less than half of total esophageal cancers.
Adenocarcinoma
Adenocarcinomas are the cancers that start in gland cells which make mucus and are the most common types of oesophageal cancers. This type of oesophageal cancer usually occurs in the lower third or distal part of the esophagus.
Adenocarcinomas that start at the gastroesophageal (GE) junction area includes about the first 2 inches (5 cm) of the stomach called the cardia and tend to behave like cancers in the esophagus. Therefore, these are also grouped with esophagus cancers.
Other less common and rare types of esophageal cancer includes lymphomas, melanomas and sarcomas.
What are the signs and symptoms of esophageal cancer?
Oesophageal cancer doesn’t manifest symptoms during its early stages and you probably will not experience any symptoms until it has progressed to advanced stage. These symptoms can also occur in many other conditions and do not necessarily mean that you have the cancer. However, you may experience any of the following signs of esophageal cancer:
- Dysphagia – difficulty swallowing, first solid foods and upon worsening even liquids are difficult to swallow
- Persistent indigestion or heartburn
- Vomiting just after having food
- Loss of appetite
- Unexplained weight loss
- Discomfort and pain in your upper tummy, chest or back
- Vomiting blood
- Black coloured or bloody stools
- Chronic cough especially while swallowing
- Hoarseness in voice
- Persistent tiredness
- Pain in your throat behind the breastbone
- Frequent choking while eating
Since esophagus is hidden within the chest cavity and is not easily evaluated by your doctor, it’s very difficult to diagnose it during routine physical examination. There are no symptoms in early stage of esophageal cancer and it appears to begin only when the tumour grows enough to cause problems.
If the cancer has spread to other parts of the body beyond the esophagus via the lymphatic system, there may be abnormal lymph nodes which can be felt or touched below the jaw in the neck region or above the clavicles (collarbones). In case the cancer has spread to the liver, it may cause liver enlargement and may be palpated on examination of the abdomen. Read about liver cancer.
What are the causes of esophageal cancer? How much do we know about the cause of esophageal cancer?
As with most cancers, it’s not exactly clear what causes esophageal cancer. However it is thought to be linked with the abnormalities, or mutations, in the DNA of the cells of the esophagus. These abnormalities and mutations provoke the cells to multiply more rapidly than normal cells and also alter the signal of their death leading to an imbalance between formation of newer cells and death of the older cells. This uncontrolled and unregulated multiplication of the cells cause them to accumulate and become tumours which can grow to invade nearby structures and spread to other parts of the body as well called metastasis.
You may develop esophageal cancer for no apparent reason but there are certain risk factors which can make you more likely to develop this cancer.
It is believed in research community that some risk factors, such as the use of tobacco or alcohol, may cause esophageal cancer by damaging the DNA of the lining cells of the esophagus. Constant exposure of the lining cells of the esophagus to irritation, as happens in case of Barrett’s esophagus, reflux, Plummer-Vinson syndrome, achalasia, or scarring from swallowing lye, may also lead to DNA damage and ultimately cause the development of cancer.
What are the risk factors of esophageal cancer?
A risk factor is anything that increases your chances of developing a disease such as a cancer. Some risk factors are under your control and you can change them such as smoking while there are others that can’t be changed, such as your age or race.
These risk factors do not directly cause the cancer but only influence the chances of someone getting the cancer. You may never develop cancer despite having several risk factors and sometimes it develops without any known risk factor being there. Just having these risk factors does not mean that you will develop the esophageal cancer.
Researchers and scientists have found several factors that can affect your risk of developing the esophageal cancer. Some of them are more likely to increase the risk for esophageal adenocarcinoma and others can put you at risk of squamous cell carcinoma of the esophagus.
Following listed factors can make you more susceptible of developing esophageal cancer.
- Age – People between age of 45-70 are at higher risk of developing this cancer
- Gender – Men are 3 times as likely to develop esophageal cancer as women
- Race – Black people are twice likely to develop squamous cell carcinoma than white people
- Tobacco chewing
- Smoking
- Heavy alcohol consumption
- Obesity / overweight
- Lye – It can cause squamous cell carcinoma as it is a corrosive chemical agent that can burn and destroy esophageal cells
- Achalasia – It increases the risk of squamous cell carcinoma
- Infection with Human pappilloma virus (HPV)
- Diet – Nutrition devoid of fruits and vegetables can increase your risk of developing this cancer
- Barrett’ s esophagus
- Gastroesophageal reflux disease (GERD)
- Having bile reflux
- Tylosis
- Plummer- Vinson Syndrome
- Exposure to certain chemicals at workplace such as solvents used in dry cleaning
- Undergoing radiation treatment for chest or upper abdomen
Gastroesophageal reflux disease and esophageal cancer
Your stomach secretes strong acids and enzymes to help in digesting the food you eat. In some instances, this acid can escape from the stomach up into the lower part of the esophagus – a condition medically known as gastroesophageal reflux disease (GERD), or just reflux. GERD is presented by the symptoms such as heartburn or pain that seem to come from the middle of the chest. However, in some people it does not manifest any symptoms at all.
GERD makes you more likely to develop esophageal adenocarcinoma and the risk seems to be higher in people who experience more frequent symptoms. Most of the people who have GERD do not develop esophageal cancer as GERD is a very common condition. However, it causes another condition known as Barrett’s esophagus which is more likely to cause development of oesophageal cancer.
Barrett’s esophagus and the cancer of esophagus
Persistent and long term reflux of the acids secreted by the stomach into the lower esophagus can damage the inner lining of the esophagus. This damage causes the replacement of squamous cells that normally line the esophagus with gland cells which are more resistant to stomach acid. This condition is known as Barrett’s esophagus.
The longer the duration of reflux, the more likely it is that you will develop Barrett’s esophagus. Barrett’s esophagus puts you at a much higher risk than people without this condition to develop esophageal adenocarcinoma. However, it doesn’t always cause cancer.
These gland cells become more abnormal with time in case of Barrett’s esophagus resulting in a condition known as dysplasia which is a pre-cancerous condition. High-grade dysplasia where the cells become entirely different in morphology is considered to be the greatest risk factor for esophageal cancer.
Use of tobacco and alcohol as a risk factor for oesophageal cancer
A major risk factor for developing esophageal cancer is the use of tobacco products such as cigarettes, cigars, pipes, and chewing tobacco.
The cancer risk increases with quantity and the duration for which these products are used. For example, a person who smokes a pack of cigarettes a day or more has at least twice the chance of getting adenocarcinoma of the esophagus than a non-smoker.
The risk of developing cancer doesn’t go away completely if you have used tobacco products for long time and then stopped. However, the risk surely goes down to some extent after you quit smoking.
Heavy alcohol drinking also increases the risk of developing esophageal cancer. It is more likely to out you at risk of getting squamous carcinoma than the risk of adenocarcinoma.
The use of tobacco products in combination with alcohol drinking raises the risk of esophageal cancer much more than using either of them alone.
Plummer-Vinson syndrome and oesophageal cancer
This is a rare syndrome, where people have webs in the upper part of the esophagus. This is also called as Paterson-Kelly syndrome. It generally happens along with anaemia, tongue irritation (glossitis), brittle fingernails, and sometimes a large thyroid gland or spleen.
It is one of the risk factors of esophageal cancer. According to estimates, about 10% of the people with this syndrome develop squamous cell cancer of the esophagus or cancer in the lower part of the throat sometime in their life. It is considered as a potential risk factor.
Achalasia and Tylosis
Achalasia is a medical condition where the muscle at the lower end of the esophagus (the lower esophageal sphincter) fails to relax properly. Food and liquid that are swallowed are not able to pass into the stomach and starts getting collected in the esophagus. This accumulation of foods and liquids result in the stretching out or dilation of lower esophagus over time. People with this condition have a risk of esophageal cancer. But cancers are found about 15 to 20 years after achalasia begins.
Tylosis is a rare and an inherited disease. In this condition, there is an excess growth of the top layer of skin especially on the palms of the hands and soles of the feet. People with this condition have a very high risk of getting squamous cell carcinoma of esophagus.
Diagnosis of esophageal cancer: What are the diagnostic tests for esophageal cancer? How is esophageal cancer diagnosed?
Your doctor may suggest for various medical tests after recording your medical history and a performing a physical examination to confirm the suspected case of oesophageal cancer. These tests are also used to evaluate if the cancer has spread to another part of the body from where it originally started. Your doctor will consider results from these tests to decide the best possible treatment according to your disease condition.
A biopsy is the only sure way to confirm whether an area of the body has cancer. But in some cases, a biopsy is not possible due to patient’s medical condition or other factors which can limit the use of biopsy. In such an instance, your doctor may suggest other tests that will help in diagnosis.
The test used to diagnose the cancer varies from person to person. There are various factors which specify the tests that should be performed to diagnose the cancer for a particular patient. These factors include:
- Signs and symptoms
- Type of cancer suspected
- Patient’s age and medical condition
- The results of earlier medical tests
Your doctor will begin testing with a physical examination, which is usually done a doctor’s office. He or she may then order one or more of the following medical tests to diagnose suspected esophageal cancer based on the physical exam.
Barium swallow test for esophageal cancer (esophagram)
A barium swallow or a barium meal involves use of a thick white liquid called barium, which is swallowed by the patient suspected of cancer. This is used to coat the walls of the esophagus before several x-rays are taken for better visualization.
This liquid is harmless and has a chalky taste. The barium coat clearly outlines the esophagus when x-rays are taken. A barium swallow test can show any abnormal areas or any blockage in your esophagus which can be a sign of cancer. But you should remember that it can’t be used to determine how far a cancer may have spread outside of the esophagus. This test is also known as esophagram.
Usually, this is the first choice of test done to see what is causing a problem with swallowing. By using this test, even small and early stage cancers can be detected. Early cancer is manifested by small round bumps called plaques while advanced cancers look like large irregular areas. These irregular areas can cause narrowing of the inside of your esophagus.
This test is quite helpful in the diagnosis of one of the serious complications of esophageal cancer called a tracheo-esophageal fistula. Tracheo-esophageal fistula occurs when the tissue between the esophagus and the trachea is destroyed by tumours, which create a hole connecting them. This causes major problems with swallowing. Anything that you swallow in can be passed from the esophagus into the windpipe and lungs. It can result in frequent coughing or even conditions such as pneumonia. Difficulties with this problem can be reduced with the help of surgery or an endoscopy procedure.
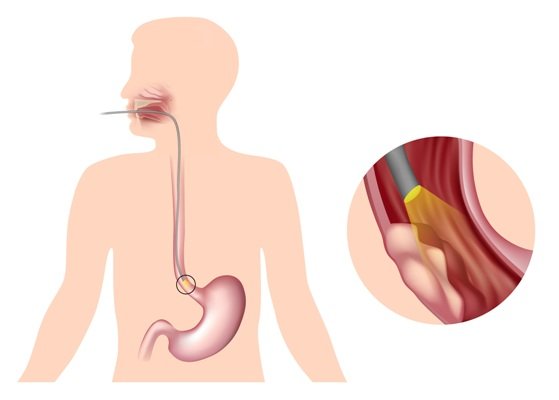
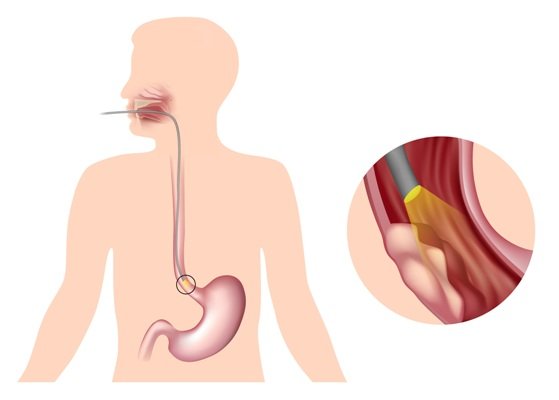
Upper endoscopy – Esophagus Gastric Duodenoscopy (EGD) for esophageal cancer
An upper endoscopy helps your doctor in viewing the lining of the esophagus. During this test, an endoscope – thin, flexible tube with a light and video camera on the end, is passed down the throat into the esophagus while you are sedated.
Sedation helps you to feel sleepy and make you calm during the procedure. Your doctor will try to look for presence of any abnormal area. If present, a biopsy will be needed to find out if it is cancerous. It can also help in widening of any blocked area of your esophagus using an inflatable balloon to stretch the esophagus. This widening will help in the passage of food until the treatment begins.
Endoscopic Ultrasound for esophageal cancer
Ultrasound uses sound waves to generate a picture of the wall of the esophagus and nearby lymph nodes and structures. During this procedure, an endoscopic probe is inserted into the esophagus through the mouth with an attached ultrasound probe that produces sound waves. The image generated by ultrasound is used to find out if the tumour has grown into the wall of the esophagus and to what extent.
This test can also be used to find out whether the cancer has spread to the lymph nodes or any other nearby structures. This procedure is often performed in succession to the upper endoscopy.
Bronchoscopy for detecting oesophageal cancer
During this procedure, the doctor passes a thin, flexible tube with a lighted head on its one end into the mouth or nose, down through the windpipe, and into the breathing passages of the lungs. It is useful if the tumour is located in the upper two-thirds of the esophagus. It can also reveal if the tumor is growing into a person’s airway. This part of a person’s airway includes the trachea, or windpipe, and the area where the windpipe branches out into the lungs called the bronchial tree.
Biopsy for diagnosing oesophageal cancer
Endoscopy and other imaging tests can suggest the presence of a cancer but only a biopsy can make a definite diagnosis. For a biopsy, your doctor will take out a small amount of tissue from the suspicious area with the help of a special instrument for further examination. These samples are then analyzed by a pathologist in the laboratory for molecular study of the tumour.
HER2 testing
If the diagnosis of esophageal cancer has been confirmed but the tumour is too advanced for surgery, your biopsy samples may be tested for the HER2 gene or protein. Some people with oesophageal cancer have elevated levels of HER2 protein on the surface of their cancer cells, which drives the cells to grow and spread rapidly. This test will help your doctor decide whether you are eligible for a target therapy-based treatment
Blood tests for oesophageal cancer
Your doctor may recommend certain blood tests to help in the diagnosis of the esophageal cancer. He/she may suggest for complete blood count test which measures the different types of cells in your blood to determine if you have anaemia. Most of the patients of esophageal cancer are found to have anaemic condition because of the excess bleeding by the tumour. You may also be required to get a liver function test done which measures the levels of liver enzymes. Esophageal cancer may spread to liver and alter your normal liver function.
Computed tomography (CT) scan for esophageal cancer diagnosis
During a CT scan, a 3-dimensional picture of the inside of the body is taken from different angles using x-rays. When these images are combined to generate a detailed and cross-sectional view, it can show the abnormalities or tumours in the body. It is also helpful in determining the size of the tumour. Usually, before performing a CT scan, a special dye called contrast medium is injected into a patient’s vein to provide better details.
Magnetic resonance imaging (MRI) for esophageal cancer
An MRI is used to produce detailed images of the body and works on the principle of magnetic fields. Sometimes, this test is also used to measure a tumour’s size. Like CT scan, a contrast medium is used in this method as well to create a clearer picture. Usually, this contrast medium is injected into a patient’s vein before performing an MRI.
Positron emission tomography (PET) scan for sophageal cancer
A PET scan is an imaging test which is used to create pictures of organs and tissues inside the body. In this procedure, first a small amount of a radioactive sugar substance is injected into the patient’s body. This radioactive substance is consumed by the cells which require higher amount of energy. Since, cancer cells use energy very actively, it absorbs more of the radioactive substance. A scanner is then used to detect the substance to produce the images. Sometimes, a PET scan is combined with a CT scan and is known as a PET-CT scan.
After performing the necessary diagnostic tests, your doctor will review the results with you. If the tests confirm an esophageal cancer, the results will be used by your doctor to associate a stage to the tumour. This process is called staging of the esophageal cancer.
Staging and grading of esophageal cancer: What are the different stages of esophageal cancer? How is staging of the esophageal cancer done?
Staging of esophageal cancer refers to the use of a system to describe the cancer location, its spread and locations where it has spread, if it has. In case of an esophageal cancer, staging usually shows how deep the cancer has extended into the esophageal tissue, whether it has spread to lymph nodes, and which other organs in the body might be involved.
These stages are determined with the help of diagnostic tests as discussed above. Staging is also useful in planning treatment option for individual patients according to the stage and condition of tumour in the esophageal tissues and to predict a patient’s prognosis and survival.
TNM staging system of oesophageal cancer
The most often used staging system for esophageal cancer is TNM system, which is developed by the American Joint Committee on Cancer (AJCC). It is based on 3 key pieces of information:
- T refers to the size and extent to which the primary tumour has grown in the esophageal wall
- N refers to the spread to lymph nodes, where and how many?
- M refers to the presence of metastases, if yes, where has it extended and to what extent?
Each letter is assigned a number to describe the esophageal cancer as follows.
Tumour (T)
- Tis – This is very early stage cancer and is called a carcinoma in situ. In this stage, the cancer cells are present only in 1 small area of the top lining of the esophagus without any spread into the lining.
- T1 – At this stage, the cancer cells have spread into the lining of the esophagus.
- T2 – The tumor has spread into the muscularis propria, which is third layer of the esophagus but not through the muscle wall of the esophagus.
- T3 – The tumor in this stage progresses to the outer layer of the esophagus called the adventitia. Also, the cancer cells have spread through the entire muscle wall of the esophagus into surrounding tissue.
- T4 – As the cancer reaches to this stage, the tumour has already spread outside the esophagus into its surrounding areas such as the windpipe, diaphragm, large blood vessel coming from the heart called the aorta, and the pleural lining of the lung.
Nodes (N)
- N0 – The cancer was not found in any lymph nodes.
- N1 – The cancer has spread to 1 or 2 lymph nodes in the chest, near the tumour.
- N2 – The cancer has spread to 3 to 6 lymph nodes in the chest, near the tumour.
- N3 – The cancer has spread to 7 or more lymph nodes in the chest, near the tumour.
Metastasis (M)
The “M” indicates whether the cancer has spread to other parts of the body. It has two stages.
- M0 – The cancer has not spread to other parts of the body.
- M1 – The cancer has spread to another part of the body.
Based on the above TNM numbers, the doctor then determines an overall stage of the cancer by assigning a simple number (I–IV). These stages (stage 1, stage 2, stage 3, and stage 4)) can be described as follows.
Stage I – This is the early stage of the cancer where the tumours are limited and found only in the esophageal wall lining.
Stages II and III – In these stages of the esophageal cancer, tumours have spread deeper into the layers of the esophageal walls and to the nearby lymph nodes. These are also known as locally advanced states of the cancer.
Stage IV – This is the advanced or metastatic stage of the esophageal cancer where the tumours have spread beyond the esophageal wall to other parts of the body and to the distant lymph nodes.
What are the grades of oesophageal cancer?
The grade of the cancer describes how closely the cancerous cells look like normal tissues when seen under a microscope. This is supposed to have an impact on the treatment and outlook of your esophageal cancer.
Grading of oesophageal cancer is done on the scale of 1 to 3.
- Grade 1 (G1) – It means the cancer cells look more like normal esophagus tissue and is well differentiated.
- Grades 2 (G2) – It is moderately differentiated condition of the cancer which falls somewhere in between G1 and G3.
- Grade 3 (G3) – It means the cancer cells look very abnormal in comparison to the normal tissues. These cells are categorized as poorly differentiated or undifferentiated.
The grading of esophageal cancer is often simplified as G1 being the low grade and G3 being the high grade. Usually, the outlook is better for low-grade cancers than it is for high-grade cancers of the same stage. Low-grade cancers are grow and spread very slowly than high-grade cancers.
Resectable versus unresectable esophageal cancer
The staging and grading of esophageal cancer as explained above are enough to provide a detailed understanding of how far an esophagus cancer has spread. But, the doctors are often more concerned about whether the cancer can be removed completely with surgery or not.
If the cancer can be removed completely by surgery, based on its location and the extent to which it has spread outside of the esophagus, the cancer is considered potentially resectable. Unresectable cancers are those which can’t be removed completely because they have spread too far in your body.
Generally, all stage 0, I, and II esophageal cancers are potentially resectable. In case of stage III cancers, most are potentially resectable even when they have spread to the nearby lymph nodes. But the stage III cancers can be resected only if the cancer has not grown into the trachea, the aorta, the spine, or other nearby important structures. However, majority of patients are not able to have surgery despite having potentially resectable cases of esophageal cancer due to poor health condition.
Oesophageal cancers that have either grown into the nearby structures or have invaded the other organs or have spread to the distant lymph nodes are considered unresectable. For unreseactable cancers, treatments other than surgery are usually considered.
What are the treatments for esophageal cancer?
Depending on the type and stage of the esophageal cancer, there are various treatment options which can be considered. These are discussed here.
Local treatments for esophageal cancer
Treatment options of this category target the tumour in a specific location without affecting the rest of the body. This is also known as local therapy for esophageal cancer. Types of local treatments used for esophageal cancer include:
- Surgery
- Radiation therapy
- Endoscopic treatments
These options are more likely to be useful for earlier stage (less advanced) cancers, although they might also be used in some other situations.
Systemic treatments for esophageal cancer
Esophageal cancer is also treated by the use of anti-cancer drugs which are administered either orally or directly into the bloodstream. These anti-cancer agents reach to the cancer cells almost anywhere in the body by travelling through your blood stream. This movement of the drugs through your whole system makes it eligible to be called as systemic treatment. The various types of systemic treatments include:
- Chemotherapy
- Targeted therapy
- Immunotherapy
In many cases, two different types of treatments are combined at the same time or used one after one another. This is determined by the stage of your cancer and various other factors. When it is difficult to remove all the cancers from the body, many of these treatments can also be used as palliative treatment.
Palliative treatment is not expected to cure the cancer but it is used to provide relief from symptoms of the cancer, such as from pain and trouble in swallowing.
Surgery for oesophageal cancer (esophagectomy etc)
Surgery used to be the most common treatment for oesophageal cancer earlier irrespective of a cancer stage, but now its use is generally limited to early stage esophageal cancer when the cancer has not spread far beyond the original tissues and it is still easy to remove the tumour surgically. During surgery, the tumour with small portion of surrounding healthy tissues is removed.
A combination of chemotherapy and radiation therapy may be used before the surgery to reduce the size of the tumour for locally-advanced esophageal cancer patients.
The most common surgical procedure to treat esophageal cancer is called an esophagectomy, where the doctor removes the affected part of the esophagus and then connects the remaining healthy part of the esophagus to the stomach so that the patient can swallow normally. This connection is made by using the stomach or some part of the intestine. Your doctor will also remove the lymph nodes around the esophagus.
Like any surgery, surgical intervention of esophageal cancer also has some complications which can be life-threatening in some cases.
Some of the risks of surgery include reactions to anesthesia, excess bleeding, blood clots in the lungs or elsewhere, and infections. You can also have lung complications which are common and may develop pneumonia also. You may also experience a voice change after the surgery.
In addition to the treatment of cancer, minor surgery can also be used as palliative care to relieve the symptoms caused by the cancer and to help patient eat properly which may include esophageal dilation and esophageal stent placement.
Radiation therapy for oesophageal cancer
Radiation therapy for esophageal cancer may be used:
- as part of the main treatment of esophageal cancer in some patients, typically along with chemo. This is often used for people who can’t have surgery due to poor health or for people who don’t want surgery.
- as neoadjuvant treatment before surgery to shrink the cancer and make it easier to remove.
- as adjuvant therapy after the surgery to kill any areas of cancer cells that may have been left behind but are too small to see.
- as palliative therapy to ease out the symptoms of advanced esophageal cancer such as pain, bleeding, or trouble in swallowing.
There are mainly two type of radiation therapy.
- External beam radiation therapy
- Internal beam radiation therapy
External beam radiation therapy is one where the radiation is focussed on the tumour from outside of the body. Another type of radiation therapy is internal beam radiation therapy where radioactive material is passed down your mouth and placed near the tumour with the help of an endoscope. The advantage with internal beam radiation therapy is that it doesn’t affect the nearby normal cells.
Some of the common side effects of the radiation therapy include nausea, vomiting, fatigue, dry mouth with thick saliva, painful sores in the mouth and throat and also skin changes such as redness, blistering and peeling.
If you experience any side effects, you should consult your doctor for symptomatic relief and inform him/her about it immediately.
Endoscopic treatments for esophageal cancer
Surgical removal of the tumour may be accomplished via endoscopic procedure if the esophageal cancer has not spread to the distant organs and the lymph nodes and is confined only in the walls of the esophagus.
Some endoscopic procedures are used to cure very early stage cancers that are not spread much into the deep tissues, or even to prevent the pre-cancers from becoming true cancers by treating such as Barrett’s esophagus or dysplasia conditions.
Endoscopic treatments are also used as palliative therapy to relieve the symptoms from late stage esophageal cancers that can’t be removed surgically. These procedures may include:
- Endoscopic mucosal resection
- Photodynamic therapy
- Radiofrequency ablation
- Laser ablation
- Argon plasma Coagulation
- Esophageal stent
Photodynamic therapy for esophageal cancer
Esophageal cancers that are small in size and have not spread or metastasized can be treated with the help of light therapy. For this therapy, a photo-sensitizing drug is injected into the body where it is absorbed by the cells, where they can last for two to three days. On exposure to light from a laser source, the drug may kill the cancer cell.
Presently, this type of treatment is limited because of the inability of light to penetrate deeply into the body. It is also thought to be effective only in case of small tumour. It is an approved therapy for esophageal cancer and non-small-cell lung cancer.
Chemotherapy for esophageal cancer
Use of drugs to destroy cancer cells is known as chemotherapy. These anti-cancer drugs usually work by stopping the cancer cells’ ability to grow and divide. It is part of systemic treatment in which chemotherapy gets into the bloodstream to reach cancer cells throughout the body. Chemotherapy is administered either orally or through intravensous (IV) route.
Chemotherapy is usually given in cycles over a given period of time which constitutes a regimen of chemotherapy. You may receive 1 drug at a time or combinations of different drugs at the same time. It may be used as a neoadjuvant therapy, an adjuvant therapy or as a standalone therapy for advanced cancers.
Various anti-cancer drugs used in case of esophageal cancer may include the following:
- Carboplatin
- Paclitaxel
- Cisplatin
- 5- fluorouracil
- Epirubicin
- Capecitabine
- Oxaliplatin
- Irinotecan
Chemotherapy has some general side effects including nausea, vomiting, loss of appetite, fatigue, hair loss, mouth sores, diarrhoea, constipation and low blood counts. Some of these agents have their specific side effects which can have long lasting effect on your body too such as Hand foot syndrome, nerve damage and allergic reactions. Thought these side effects go away once the treatment is complete, but some may last long.
Targeted therapy for esophageal cancer
This treatment approach targets the specific genes, proteins, or the cellular environment that contributes to the cancer growth and survival of the particular cancer. Targeted therapy effectively blocks the growth and spread of cancer cells while limiting the damage to healthy cells of your body.
To target the specific genes or proteins, your doctor may suggest some tests to identify the genes, proteins, and other factors in your tumour. This also helps your doctor decide the most effective treatment according to your need. Many researchers are engaged in studies to find more about specific molecular targets of the cancers and new treatments directed at them.
Targeted therapy for esophageal cancer includes a drug trastuzumab or herceptin which targets the HER2 protien. Another example of targeted therapy is ramucirumab which block the formation of new blood vessels in the tumours to cut the supply of nutrients to the cancerous cells. This is also known as anti- angiogenesis therapy.
Immunotherapy for oesophageal cancer
Immunotherapy refers to the use of medicines that drive your own immune system to find and destroy the cancer cells. It can be used to strengthen the immune system of some patients having esophageal cancer.
Pembrolizumab is a medicine which is used in some people with advanced cancer of the gastroesophageal junction who have had tried other treatment options earlier, which did not help. It blocks PD-1 which is a protein on the T cells of the immune system and boosts the immune response against cancer cells.
This is also helpful in slowing the growth of tumours and their shrinkage. It is administered as intravenous infusion after every 3 weeks. You may experience infusion reaction and autoimmune reaction as the side effects of this therapy which can be life-threatening as well in some cases. It is important to discuss risks and benefits with your doctor before starting immunotherapy.
Possible side effects of this drug include:
- Nausea
- Shortness of breath
- Feeling tired or weak
- Fever
- Cough
- Loss of appetite
- Itching
- Skin rash
- Muscle or joint pain
- Constipation or diarrhoea
What is the prognosis with esophageal cancer? What is the survival rate for esophageal cancer?
Usually, treatment for esophageal cancer is possible but it is not a curable disease because it gets diagnosed in advanced stage generally, when surgical resection of tumour is not possible.
However, patients who have severe Barrett’s esophagus, which is also considered to be the stage T0 or pre-cancerous stage and those with few cancer cells tend to have relatively successful outcomes.
The estimated overall five-year survival rate for esophageal cancer according to the National Cancer Institute is about 18.8%. This survival figure is considered to be low because generally patients tend to develop symptoms and signs late in their disease when the cancer has already spread to nearby tissues or to the distant organs and lymph nodes.
Patients whose tumours disappeared with radiation and chemotherapy before surgery have better survival rates and it is reported to be 48% for three year survival rate. Whereas, the three year survival rate for the patients who had some residual tumour at the time of surgery significantly reduced to 27%.
Squamous cell carcinoma and adenocarcinoma of oesophageal cancer have almost similar prognosis.
The typical five year survival rate for esophageal cancer is:
- For localized esophagus cancer that hasn’t spread from its primary site, survival rate is 42.9%,
- For esophageal cancer with regional spread, the survival rate is 23.4%
- For esophageal cancer with distant metastasis, the survival rate is 4.6%
- For esophageal cancer with unknown staging, the survival rate is 12.4%
Is it possible to prevent esophageal cancer? How can you prevent esophageal cancer?
It is not possible to prevent all oesophageal cancer cases. But you can greatly reduce the risk of developing this cancer by avoiding certain high grade risk factors which may include:
Avoiding tobacco and alcohol
Use of tobacco products and heavy alcohol drinking are the most important lifestyle risk factors for cancer of the esophagus. Both of them are thought to increases the risk of esophageal cancer many folds, and the risk is even greater if they are combined. You can avoid the risk of developing esophageal cancer by avoiding the use of tobacco and alcohol drinking.
Getting treated for reflux or Barrett’s esophagus
People with Barrett’s esophagus are at higher risk for esophageal cancer. Treatment of this condition usually prevents the development of cancer in the esophagus. People who have this condition are often monitored for signs indicative of the lining cells of the esophagus to have become more abnormal.
If needed your doctor may recommend surgery for the treatment of the Barrett’s esophagus to keep it from developing into esophageal cancer.
Watching your diet and body weight
Eating a healthy diet rich in fruits and vegetables may help protect against esophageal cancer. Obesity is one of the risk factors for developing esophageal cancer, particularly the adenocarcinoma. Therefore, staying at a healthy weight may also help limit the risk of this disease.
Can you get second cancer after successful treatment of esophageal cancer?
The greatest concern of a cancer survivor is facing cancer again besides other health problems due to treatment of the esophageal cancer earlier. Coming back of the cancer after successful treatment is called “recurrence.”
Some patients may even develop a new, un-related type of cancer later which is called a “second cancer.” There is a high possibility of you getting the second cancer after surviving the earlier one, no matter what type of cancer you have had earlier.
Esophageal cancer survivors have increased risk of getting the following types of second cancer.
- Cancer of the larynx (voice box)
- Cancers of the mouth and throat
- Lung cancer
- Stomach and small intestine cancer
- Thyroid cancer












