Eye Cancer (Ocular Cancer): Causes, Symptoms, Types, Stages, Risks, Treatment, Prevention
- Updated on: Jul 10, 2024
- 26 min Read
- Published on Sep 27, 2019

What is Eye Cancer (Ocular Cancer or Eye Neoplasm)?
Cancer begins when cells in the body begin to grow in an uncontrolled manner. Cells in almost any part of our body can become cancer, and can spread to other areas of the body. An eye cancer is such an uncontrolled growth that starts in the eye.
When cells grow in an abnormal fashion forming tumor in any part of the eye leading to the loss of vision, it turns to be the beginning of eye cancer. Tumors can be both benign i.e. it does not spread and malignant i.e. it grows and spreads to other parts of the body.
Eye Cancer or eye neoplasm is a rare disease. It generally spreads to the eye from another organ like skin or lymph nodes and is known as secondary eye cancer, which is more common than the primary eye cancer. A primary eye cancer is the one that originally starts from the eye. This article is focused on primary eye cancer.
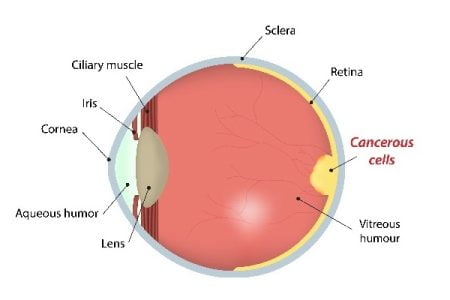
What are the different parts of the eye?
Eyeball
The eyeball also known as globe of the eye is the main part of human eye. It consists three different layers:
- Sclera: It is the outer fibrous layer and helps maintain the shape of the eye.
- Middle blood rich layer called Choroid: It is the layer in eye where the blood vessels carry food and oxygen for the eye.
- Inner pigmented nerve layer called retina: It is light sensitive and it sends message to the optic nerve to make it possible to see.
The inside of the eyeball is filled with a jelly like substance called as Vitreous Humor. The covering of the front of the eye ball is called Conjunctiva.
The Uvea
It is the combination of Iris (manages the amount of light entering the eye) and Ciliary body (keeps the eye moist with the help of cells secreting aqueous Humor and maintains eye focus).
Orbit (Eye Socket)
The orbit comprises of tissues surrounding the eyeball. These include muscles that move the eyeball in different directions and the nerves attached to the eye.
There are other accessory (adnexal) glands present around the eye such as tear glands and eyelids.
Types of Eye Cancer
Eye cancer, in medical terminology, is known as Ocular Cancer. There are primarily two types of eye cancers:
- Primary eye cancer: It starts from the eye i.e. It is also called intraocular cancer.
- Secondary eye cancer: It starts somewhere else in the body and then spread to the eye from there.
Primary eye cancer (intraocular eye cancer)
As mentioned above, it starts from the eye. There are several types of primary intraocular cancer. In adults, melanoma is the most common primary intraocular cancer, followed by primary intraocular lymphoma.
The various types of primary eye cancer are discussed herein:
Melanoma
Melanoma is the most common type of intraocular eye cancer that develops in melanocytes of the eye. Melanocytes are cells that make pigment or provide coloring in eye, skin, lips, etc.
Melanoma growing in the eyeball is unusual, but it is the most general type of eye cancer in adults. In about 8 of 10 cases of primary eye cancers are of this type. Melanomas often bud in uvea or iris of the eye, and therefore are known as Uveal Melanomas.
Intraocular melanomas are of two kinds based on the cells they occur in. The two types of cells are:
- Spindle cells: These are thin, stretched out and long cells.
- Epithelioid cells: They are oval- or spherical-shaped cells but with some straight edges i.e. non-spindle structures.
There are no early signs or symptoms of melanoma and it can only be defined through medical examination.
Lymphoma
Lymphoma begins in the immune system cells called lymphocytes. Lymphoma can begin in any internal organ of the body where lymph nodes, bean sized collections of lymphocytes, are present.
Lymphoma is mainly of two types:
- Hodgkin lymphoma also called Hodgkin disease: Hodgkin lymphoma most commonly affects lymph nodes in the neck or in the area between the lungs and behind the breastbone. It can also initiate in groups of lymph nodes under an arm, in the groin, or in the abdomen or pelvis.
- Non-Hodgkin lymphoma: It begins anywhere in stretches (in size), to almost any organ. It commonly starts in the lymph nodes, spleen, liver, or bone marrow. In addition, it can involve stomach, intestines, skin, thyroid gland, brain, or any other part of the body.
Very rarely lymphoma begins inside the eyes. But if it does, it is called primary intraocular lymphoma. Primary intraocular lymphomas are always a type of non Hodgkin lymphoma. You are more likely to have intraocular lymphoma if you have a weak immune system.
Retinoblastoma
Retinoblastoma is an eye cancer that begins in the retina. It rarely spreads to other parts of the body.
The retina is a thin layer of nerve tissue that lines the inside of the back of the eye and is sensitive to light. As the retina senses light, it sends a message by way of the optic nerve to the brain, in order to capture the view. The formation of malignant cells in the tissues of the retina is known as Retinoblastoma.
Retinoblastoma is a rare children disease occurring at the age of about 5. A study shows that about 200–300 children are diagnosed with this disease in the US and most of them are below 3 years of age.
Orbital and adnexal cancers
Tissues of muscles, nerves, and skin around the eyeball and their counterparts in other parts of the body develop cancers of the orbit and adnexa.
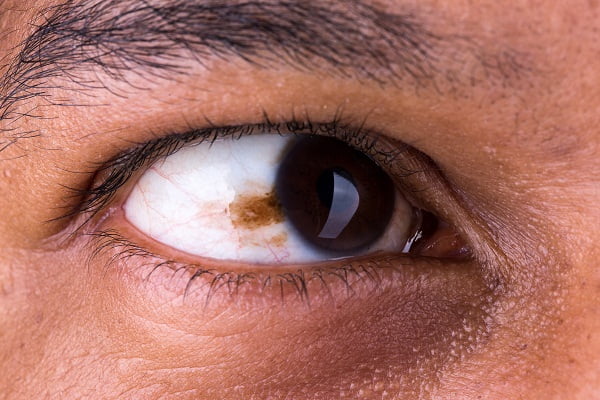
Conjunctival melanoma
It is a tumor of the conjunctiva, which is a membrane that lines the eyelid and eyeball. A dark spot occurs in the eye on the conjunctiva which is supposed to be a tumor and has a tendency to reoccur.
Eyelid cancer
The most common types of cancer occurring on the eyelid are basal or squamous cell cancer, which are variants of the skin cancer.
Squamous cells are flat and low grade cells which spread at a very low rate around the eye. Eyelid cancer usually grows on the surface of the conjunctiva but can grow into and around the eye too.
Secondary eye cancer
Sometimes, cancer can spread to the eye from another part of the body and is not truly ‘eye cancer’. In women, the secondary eye cancer commonly occurs with breast cancer (carcinoma), and in men, it occurs with lung cancer generally affecting the uvea of the eyeball.
Risk factors and Causes of Eye cancer
What causes eye cancer? Do we know about the cause of eye cancer?
The exact cause of most eye cancers is not known. Scientists are researching to identify how certain changes in the DNA and genetic mutations inside the cells can cause the cells to become cancerous and possibly work as potential eye cancer causes.
DNA is the chemical and genetic basic unit in each of our cells that forms our genes and genetic structure and the instructions for how our cells function. Scientists believe that DNA can also influence the risk for developing certain types of cancer and act as potential eye cancer causes.
The genes in the cells are the key-players. They manage the cell division and growth. This division is controlled by tumor suppressor genes who at the right time lead to the death of the cells which are not required.
The cancer causing genes, known as the oncogenes , turn off the tumor suppressor genes which leads to excessive cell division forming outgrowth known as tumors. For example, changes (mutation) in the BAP1 tumor suppressor genes increase the risk of eye melanoma and some other cancers as after mutation BAP1 doesn’t work normally, which can allow cells to grow out of control.
Another recent research portrayed that about 4 out of 5 eye melanomas have changes in any of the two related genes, GNA11 or GNAQ, which appear to be oncogenes leading to the eye cancer. This hints to more types of eye cancer causes.
Researchers are studying these and other DNA (genetic) changes to understand more about them and how they might cause eye cancer of various kinds. But it is still not completely clear what causes these changes to occur in some people and not others. However, they define certain risk factors that increase the chances of developing a cancer of certain type.
What are the risk factors for various types of eye cancer?
A risk factor for eye cancer is something that affects your chance of getting the eye cancer. Not all types of cancers have same risk factors.
Having a known risk factor, or even many risk factors, does not mean that you will get the eye cancer. Many people who get the eye cancer may have few or no known risk factors at all.
Common eye cancer risk factors are listed herein.
Exposure to harmful radiations
- Extreme exposure to sunlight can lead to melanoma of skin. Exposure to chemicals or UV radiations, for example working with sunbeds (artificial UV radiations), can lead to severe skin cancer (including in or around the eye).
- High-energy radiation, such as x-rays, gamma rays, alpha particles, beta particles, and neutrons, damage the DNA and cause cancer.
- Highly valued medical procedures, such as computed tomography (CT) scans, positron emission tomography (PET) scans, MRI and other radiation therapies can also become a reason for the commencement of the eye cancer, but very rarely.
Age, Gender and Eye Color
- An analysis from NCI’s surveillance, epidemiology, and end results program provided a statistical data stating that eye cancer is most likely to occur after 65 years of age.
- Eye melanoma is more common in men than in women.
- People with light colored eye have more chances to develop eye cancer than people with dark colored eyes.
Family history
- Although it is rare, but sometimes due to mutation or any change in the gene called BAP1, the risk of eye (uveal) cancer increases in the family.
- Around 4 out of 10 retinoblastoma (40%) can prevail in the family. Mutation occurs by birth in a few children in the retinoblastoma gene (RB1 gene) which they inhibit from their parents.
Individual Lifestyle
- The consumption of alcohol or tobacco is one major reason why cancer is growing at a very high rate.
- A proper diet with minerals and antioxidants help to boost the immune system, thus preventing the damage caused by external agents to the DNA.
- HIV also weakens the eye muscles and immune system and therefore the chances become higher for any cancerous cell to grow in the body.
- During pregnancy, if the mother smokes, the child suffers with high risk of retinoblastoma.
- People who take anti-rejection drugs after any organ transplant surgery are also subjected to eye cancer risk.
Prevention of Eye cancer
Eye is one of the most sensitive body parts. Regular checkups are important for people who suffer with severe eye diseases, even if there are no early symptoms. Often melanomas are detected during routine eye examinations.
The American Cancer Society recommended wearing UV-protected sunglasses in strong sunlight when moving outside. About 99% of UVA and UVB are absorbed through it which not only protect the eye but also the area around it.
The risk of eye infection should be extremely avoided as it increases the chance of spread of HIV which causes the deterioration of vision and development of tumors in the lymph nodes. This can easily lead to eye lymphoma.
There is no known method of preventing eye cancers but people may be able to reduce their risk of getting it.
Early signs, symptoms, and detection of eye cancer
There is no widely recommended screening test for the detection of eye cancer but regular eye checkups can help in reducing the risk of severe eye cancer.
Most of the times, ophthalmologists find melanoma through regular eye examinations although it is difficult to detect it at an early stage. Ophthalmologist examines through the pupil at the back of the eye, where dark spots might appear, which can be an early melanoma.
It is often seen that most eye melanomas begin with a mole, called nevus, in the eye which is a benign tumor progression of pigmented cells in the eye.
What are the common signs and symptoms of eye cancer?
The symptoms are not very obvious until the cancer reaches the latter stage. Still, these are considered to be the common signs of eye cancer:
- The most common symptom is blurring or loss of vision
- A dark spot in the eye that gets bigger
- A displacement of the eye within the eye socket
- Visibility decreases during flashing lights
- Bulging of one’s eye and watery eyes are other symptoms which indicate the early stage of cancer development
- Floaters, or small specks or squiggles might also move about in the patient’s field of vision. Floaters are common in old age people and might not be considered a sign of cancer.
- Red eye, irritation in the eye or inflammation on the conjunctiva (conjunctivitis).
Stages of eye cancer
Once a patient is diagnosed with eye cancer, doctors try to identify if it has spread, and if so, how far and to which locations. This method is called staging of the cancer. The stage of a cancer describes how much cancer has spread in the body. The higher the stage, the more is its spread. The stage of a cancer helps doctors determine how serious the cancer is and what could be possible and suitable treatment options in that stage.
Most cases of eye melanomas start in the uvea, which includes the iris, ciliary body, and choroid. The staging of these uveal melanomas is generally done through a system called AJCC TNM staging system or TNM (Tumor Node Metastasis) System.
Another methodology devised for staging eye cancer is Collaborative Ocular Melanoma Study (COMS) staging of melanoma of the eye.
Intraocular lymphoma does not have its own staging system and, therefore, can be described with the help of Non-Hodgkin staging system.
The following staging notations are described in accordance with the TNM staging system.
AJCC TNM staging system for melanoma of the eye or TNM (Tumor Node Metastasis) staging system
The stage determination of eye cancer is based on three factors:
- The size and extent of the main tumor (T)
- The spread to nearby lymph nodes (N)
- The spread (metastasis) to distant sites (M) – metastatic cancer
The size and extent of the Tumor: T categories for iris melanoma
Different types of T categories exist for iris, ciliary body, and choroidal melanomas. As the numbers or letters increase, the stages also advance.
TX: No information is known and therefore primary tumor cannot be accessed.
T0: No proof or confirmation of primary tumor.
T1: It marks the beginning of the tumor in the iris.
- T1a: Tumor inside the iris touches 1/4 or less of it.
- T1b: Tumor touches more than 1/4 of the iris.
- T1c: Tumor is only in the iris but causes a raise in the eye pressure (glaucoma).
T2: Tumor begins growing in the ciliary body and choroid.
- T2a: Tumor grows into the ciliary body.
- T2b: Tumor expands into the ciliary body and choroid.
- T2c: Tumor maturing into the ciliary body, choroid, or both, begins to cause glaucoma.
T3: Tumor is fully-grown into the ciliary body and/or choroid and into the sclera.
T4: Tumor starts to expand outside of the eyeball.
- T4a: 5 millimeters (mm) of the tumor is outside the eyeball.
- T4b: About 1/5 inch of the tumor spreads across which is greater than 5mm in size.
T categories for ciliary body and choroidal melanoma
Ciliary body and choroidal melanomas are divided into 4 main T categories (T1 to T4) and then into subcategories, on the basis of diameter (width) and the thickness of the tumor. The smallest are the T1 tumors and the largest are T4 tumors.
TX: No known information about the tumors.
T0: No instance of primary tumor.
T1/T2/T3/T4 tumors:
- T1a/T2a/T3a/T4a: Tumor is neither growing into the ciliary body nor outside the eyeball.
- T1b/T2b/T3b/T4b: Tumor starts budding into the ciliary body.
- T1c/T2c/T3c/T4c: Tumor does not grow into the ciliary body but outside of the eyeball. The size of the tumor outside is 5mm approximately or less.
- T1d/T2d/T3d/T4d: Tumor expands into the ciliary body and also outside of the eyeball. Tumor fraction outside the eyeball is of about 5mm.
- T4e: this tumor can be of any size. The tumor keeps growing outside the eyeball with an increasing width of 5mm.
N categories for iris, ciliary body, and choroidal melanomas
The spreading out of tumor to the lymph nodes (N)
NX: Lymph nodes are not accessible.
N0: Cancer has not extended close to lymph nodes.
N1: Cancer has spread as small deposits to close lymph nodes in other parts of the eye.
- N1a: Cancer has grown to nearby lymph nodes.
- N1b: Small cancer deposits in other parts of the eye.
M categories for iris, ciliary body, and choroidal melanomas
The extension (metastasis) of the tumor cells or cancer to distance parts of the body (M).
M0: No expansion to various parts of the body.
M1: Cancer has spread to distant parts of the body.
- M1a: The largest spread area of cancer is about 3 centimeters (cm).
- M1b: The maximum area of cancer stretch is between 3.1 and 8 cm across.
- M1c: The major area of cancer spread is 8.1 cm or more across.
Stage grouping and grading of eye cancer
For assigning an overall stage, the T, N, and M categories are collected in a process called stage grouping. The stages are described by Roman numerals from I (the least advanced) to IV (the most advanced). Some stages are further divided with letters.
Collaborative Ocular Melanoma Study (COMS) staging system of the eye cancer
Doctors decide the stage of the cancer according to the width and thickness of the tumor. The stages are defined as:
- Small – the melanoma is less than 3 mm thick and not more than 10 mm wide.
- Medium – the thickness of the melanoma is between 3 and 8 mm, and wider from 10-15mm.
- Large – the melanoma is larger than 8 mm in thickness or wider than 16mm.
Staging of advanced eye melanoma
The stages of melanoma in eye, if not treated, advance with time. It reaches either of the two conditions:
- Cancer grows into the tissues near the eye
- Even after the complete treatment, cancer returns back affecting any other part of the body.
Staging of intraocular lymphoma: Non-Hodgkin Lymphoma staging system (NHL)
The present staging system used for Non-Hodgkin Lymphoma is known as the Lugano classification, which works on the basis of the older Ann Arbor system. Although, it only works for the lymph nodes and if the disease is affecting the blood or bone marrow, it is often staged using the system called SLL (Small Lymphocytic Lymphoma).
The stages of NHL by Lugano Classification include:
Stage I:
This stage signifies that either lymphoma is present only in one lymph node area or lymphoid organ for example the tonsils (I) or the cancer is established only in one area of a single organ outside of the lymph system (IE).
Stage II
There are again two conditions in this stage as follows:
- Lymphoma is in two or more groups of lymph nodes on the similar side of the diaphragm. Diaphragm is a thin band of muscle that separates the chest and the abdomen. For example, this might include nodes in the underarm and neck area but not the combination of underarm and groin nodes (II).
- Lymphoma is in a cluster of lymph node(s) and in one area of a nearby organ. It possibly will also affect other groups of lymph nodes on the very side of the diaphragm.
Stage III
Either of these two describes this stage 3:
- The lymphoma is in lymph node areas on both sides of (above and below) the diaphragm
- It is in the lymph nodes above the diaphragm, as well as in the spleen.
Stage IV
Lymphoma, at this severe stage, spreads quickly to other organs of the body like bone marrow, liver, etc apart from the lymph system.
How can staging of intraocular cancer affect the treatment plan?
The stage of a lymphoma is considered significant for the purpose of your treatment. For different stages, the treatment plan differs. The doctor would like to know whether the stage is “limited” (stage I or the beginning of stage II) or advanced” (stage III or IV) before initiating any treatment.
For example, for stage II, there are certain prognostic factors which mediate the process of treatment according to the severity of the stage.
Grading system of eye cancer
Grades (G) define that how much healthy the cancer cells look like when viewed under the microscope. The cancer can appear similar to a healthy tissue and contain different cell groupings, which is known as differentiated or a low-grade tumor. Or else, the cancerous tissue may appear very different from the healthy tissue, and is called as poorly differentiated or a high-grade tumor.
After biopsy, the tumor cells are obtained in different histological patterns, as follows:
- Spindle cell melanoma (the cells are longer and tapered at the ends)
- Epithelioid melanoma (the cells are oval-shaped)
- Mixed cell melanoma (both spindle and epithelioid)
The lower grade generally indicates a better eye cancer prognosis than a higher grade eye cancer prognosis. The terminology used for eye cancer grading is:
GX: Grade cannot be evaluated
G1: A spindle cell melanoma
G2: A mixed cell melanoma
G3: An epithelioid melanoma
The grades indicate that a tumor made up of spindle cells has a better prognosis than a tumor made up of epithelioid cells.
Ocular cancer survival rate (Eye cancer survival rate)
The survival rate of eye cancer depends on several different factors and therefore no exact detail can be provided about it. It depends on the stage of cancer, level of fitness, individual habits, type of cancer, etc.
The statistical data doesn’t help an individual to judge the intensity of his or her disease. Although for records, the onco-ophthalmologists use a ‘5-year survival plan’, but it is a relative estimation based on the percentage of people who live at least five years after the diagnosis of the disease and cannot be used to define the survival rate for an individual.
In a general study, people with eye cancer in England, the following survival rates were estimated which signify the pattern in the overall population under study:
- 95 out of every 100 (95%) survived their cancer for 1 year or more after they are diagnosed
- 70 out of every 100 (70%) survived their cancer for 5 years or more after diagnosis, and
- 60 out of every 100 (60%) survived their cancer for even 10 years or more after they are diagnosed.
Diagnosis is an important factor to determine the survival rate. The earlier the cancer is diagnosed, the better are the chances of survival. Another factor is the type of eye cancer which can also affect the survival duration for a patient.
Ocular melanoma survival rate
When the cancer is restricted to the eye, the 5-year relative survival rate of melanoma eye cancer is approximately 80%. If the eye melanomas have spread to distant parts of the body, the 5-year relative survival rate is about 15%.
Accurate survival is hard to determine because it is fairly rare but tend to be better in earlier stages than in latter stages.
Lymphoma of the eye survival rate (eye lymphoma prognosis)
Lymphoma also has almost the same prognosis. If it is diagnosed at an early stage, it is treated easily. As it is a rare condition, it is not easy to find the exact survival rate for lymphoma.
Detection and Diagnosis of eye cancer
Early detection and diagnosis of ocular cancer is important for its treatment. The signs and symptoms are the best ways to identify the beginning of an eye cancer. In addition, there are several other ways for the detection of eye cancer in early stages.
Can Eye Cancer Be Found Early?
Screening is the process of testing for a cancer or any other disease in people before any symptoms occur. Eye cancer is not a common cancer, and there are no established screening tests for this type of cancer. Moreover, the early signs of eye cancer can resemble other common eye problems. But, still, some eye cancers can be found early.
What can be done to help detect eye cancer at early stage?
Some doctors recommend yearly eye examinations for people who are at an increased risk of eye cancer particular eye melanoma. These people may include such as patients of dysplastic nevus syndrome etc. Generally, eye melanomas are detected in a routine eye exam. The doctor may see them as dark spots as they are in the early stage of development.
Many doctors feel that most melanomas start from a nevus (mole), which is a benign (non-cancerous) tumor of pigment cells. Therefore, if a doctor finds an eye nevus, he or she may investigate it further and review its condition regularly. A dark spot on the colored part of the eye (called the iris) may also indicate an early stage of the eye cancer. This should be checked by a doctor.
What are the ways to diagnose eye cancer?
Eye examination
The symptoms can enable a doctor determine whether the patient is suffering with any eye disorder and whether it can be a cancer. The blurring of vision indicates an immediate eye examination is needed. The vision and the movement of eye tell a lot about the health of the eye.
Medical (fine needle) biopsy
The procedure is referred to as Vitrectomy. A sample of vitreous gel is extracted from the eye by inserting a small instrument, which includes a fine thin needle, in the vitreous humor. The cells obtained in the form of gel are then sent to a laboratory for testing. If the tumor is found to be present in the gel, the cancerous cells are removed using a needle.
Other types of medical biopsy are:
Core biopsy: The removal of tissue with a larger core is done using a wide needle.
Incisional biopsy: The removal of a small part of the lump or a small sample of the tissue that doesn’t look normal is taken in this procedure.
Excisional biopsy: The removal of an entire lump or area of the tissue that doesn’t look normal is taken. The excisional biopsy is a more involved procedure where the entire abnormality or the target site is removed for examination.
Imaging tests (PET, MRI, CT, ultrasound)
The following imaging tests can be done to determine the shape and size of the tumor in the eye.
- Ultrasound: It helps determine the shape and size of the tumor in the eye and uses sound waves to create a picture of the eye which can be visualized on a computer sscreen.
- Positron-emission tomography (PET): A PET scan helps to indicate whether the cancer has spread to lymph nodes or other parts of the body. A PET scan can also be useful if there is any indication of the cancer to have spread but the areas of extension are not clear. A very small amount of radioactive sugar is injected into the body which is consumed by the cells that use the most energy. A scanner detects the cells which absorb maximum energy and produces an image of the area.
- Magnetic Resonance imaging (MRI): Magnetic Resonance imaging is often done to see through the areas around the eye, in the brain, or in the meninges thin layers of tissues that cover the brain and spinal cord. This technique uses magnetic fields and not x-rays, to produce detailed images of the body and also measure the size of the tumor. A special dye can be injected into a patient’s vein or given as a pill to swallow to get a clearer distinct picture before the procedure is done.
- Computed tomography (CT or CAT) scan: It shows the 3D cross-sectional picture of the body. CT scans are used comparatively less often than MRI scans for eye lymphoma as they do not provide as specific details as an MRI can do.
Cytogenetics and gene expression profiling
The analysis of a cell’s chromosomes (strands of DNA), which include the number, size, shape, and arrangement of the chromosomes is termed as Cytogenetics. Gene expression profiling test identifies specific genes, proteins, and other factors exclusive to the tumor.
These tests are basically performed to check the chances of recovery and treatment from the eye cancer.
Fluorescein angiography
A fluorescent greenish-yellow, indocyanine green, dye is injected into the vein of the patient’s arm. The dye circulates through the body and into the blood vessels in the back of the eye and a special camera is used to click quick pictures of these blood vessels in the retina. This tells the presence or absence of the tumor formation in the eye.
Treatment of eye cancer (intraocular cancer)
After diagnosis and staging of the eye cancer, a team of ophthalmologists, oncologists or ocular oncologists, radio-oncologists, will devise a treatment plan which considers patient’s health history, the type and stage of the eye cancer, the location of the cancer, etc.
Depending on the type and stage of the cancer and other factors, the various treatment options that can be used for eye cancer treatment are:
Surgery for eye cancer
Tumor resection is to remove a tumor through surgery. There is a great risk of cancer cells breaking away from the tumor and floating into the surrounding eye tissue as the operation involves opening of the eyeball.
The sclera is then placed back in the eye after the removal of the tumor. The exact surgical approach your doctor will follow depends on the location as well as the size of the tumor.
Risks with eye cancer surgery
During the operation for eye cancer, there is a risk of:
- retina becoming detached (detached retina)
- damage to the lens of the eye, causing cataracts
- bleeding (hemorrhage)
The stage of your eye cancer signifies the severity of the disease and the way the operations are performed to remove the cancer and regain the vision. Sometimes, only a part of the eye has to be removed, whereas, there are certain situations that require the removal of whole eye.
Removal of a part of the eye for treating eye cancer
Iridectomy: Removal of a small part of the iris (the colored part of the eye) which contains the melanoma.
Iridotrabeculectomy: Removing a part of the iris with a small piece of the outer part of the eyeball. This technique is useful for minor melanomas.
Iridocyclectomy: Removing of a portion of the iris and the ciliary body. This surgery is also done for small melanomas.
Choroidectomy: This surgery includes removal of a part of the choroid (pigmented, vascular part of the eye), and at times the wall of the eye too. This surgery may include some steps of radiotherapy.
Trans-scleral resection: Surgical removal of the melanoma of the ciliary body or choroid as it is hard to remove the tumor behind eye (mass behind eye or growth behind eye) without causing any damage to the rest of the eye. This could lead to severe vision problems.
Removal of the whole eye for cancer treatment surgery (Enucleation)
Enucleation: It is the removal of the entire eyeball. It is done for critical and larger melanomas of the eye, but it may also be done for some smaller melanomas if the vision in the eye has already been lost or if it is so blur that other treatment options would destroy the useful vision in the eye.
During the operation, a permanent eye implant is inserted into the socket. Orbital implant (made of silicon or hydroxyapatite) is generally placed instead of the eyeball. It is attached to the muscles that move the eye so that it moves like a normal eye moves. Within a few weeks after the surgery, an artificial eye (a thin shell) is placed that fits over the orbital implant and under the eyelids.
Orbital exenteration: This is a rare surgery which involves removal of the eyeball and some surrounding structures such as parts of the eyelid and muscles, nerves, and other tissues inside the eye socket.
This method of treatment is only used for eye melanomas which have grown outside the eyeball into nearby structures. The eye is replaced with a prosthetic version, and the muscles are reattached to allow some level of normal movement. As with enucleation, an artificial eye (prosthesis) might be placed in the socket after the surgery.
Radiation therapy for eye cancer
Radiation therapy is the use of high-energy x-rays or other particles to demolish cancer cells by destroying their genetic material. It is generally used for the treatment of small sized eye tumors.
With radiotherapy, the vision is restored (saved) but sometimes it may cause some damage to the other parts of the eye. An advantage of radiation therapy over surgery is that the eye structure remains preserved, which results in better appearance after the treatment.
Radiotherapy can also cause an increase in pressure within the eye (glaucoma) when large doses are used. Radiotherapy treatment for Non Hodgkin lymphoma usually includes both the eyes and the brain as there is a high chance of the cancer being present in both the eyes.
Types of Radiotherapy for eye cancer
Brachytherapy (episcleral plaque therapy): It is the most common radiation treatment for most eye melanomas. It is as effective as surgery in some cases. Small pellets (sometimes called seeds) of radioactive material are placed directly into or very close to the cancer. This is done when the tumor is not very thick.
The oncologists sew plaques in place alongside your eye tumor. The plaques have a lining of radioactive material, containing several iodine-125 seeds to the wall of the eye, near the tumor. It remains there for 4 to 5 days. Gold is used to shield other tissues from the radiation. This treatment cures about 9 out of 10 small tumors and can preserve vision in some patients, depending on what part of the eye the melanoma is in.
External beam radiation therapy: The most common type of radiation treatment is external-beam radiation therapy, which involves radiations given from a machine outside the body after enucleation or as a palliative treatment.
It is supposed to be best for the treatment of eye lymphomas. There are two technologies to use external beam radiation therapy, as follows:
- Conformal proton beam radiotherapy: Instead of x-rays, this method focuses proton beam on the cancer. The advantage of this method is that it delivers more radiations and does and less harm to the normal tissues around the affected area. This is a non-painful procedure. The only demerit is that it is a very costly procedure and therefore only limited users in United States are making use of it.
- Stereotactic radiosurgery: This method of treatment delivers a large, precise radiation dose to the tumor area in a single session with two different approaches. One, focusing hundreds of radiation beams of different angles at the tumor for a short period of time. The machine used to deliver this type of radiation is known as a Gamma Knife. Two, a movable linear accelerator circulates around the head to deliver radiations to the tumor from many different angles, which is controlled by a computer.
Laser therapy for eye cancer
Highly focused beams of light that can be used to destroy body tissues are known as Lasers. Laser therapy is sometimes used to treat intraocular (eye) melanoma, but not lymphoma. This therapy has fewer side effects as compared to surgery or radiation therapy. There might be some visual loss due to laser therapy.
Types of laser therapies for eye cancer treatment
- Transpupillary thermotherapy (TTT): It is an infrared laser therapy which uses heat in the form of laser to shrink the tumor and then kill it. It is best for small choroidal melanomas as laser might not be able to reach the deepest parts of large melanomas. It is not considered as the main method of treatment but as an additional treatment to radiotherapy.
- Laser photocoagulation: This therapy involves high beams which target to burn tissues. It is best in the treatment of tiny retinoblastomas and small melanomas of the eye. It takes approximately 7 weeks to treat a tumor.
Chemotherapy for eye cancer
The ingestion of cytotoxic drugs (chemo) to treat cancer is chemotherapy. The drug is taken in either by injecting in the vein (intravenous) or directly to the organ or taken orally through mouth.
It is best for treating intraocular eye lymphoma or retinoblastoma and sometimes for choroidal metastasis, conjunctival tumors, and metastatic choroidal melanoma. There are several chemotherapeutic drugs available for treating eye cancer. Each type of drug has potential side effects such as skin problems, nausea, vomiting, and infections.
There are several ways chemo can be given to patients:
Chemotherapy into your bloodstream
The drug is injected into the bloodstream through a cannula (a thin tube). This is beneficial in case when the cancer has spread to other parts of the body. It is known to be a systemic approach.
Chemotherapy into the fluid around your spinal cord
It is known as Intrathecal approach. Here, the drug is injected into the cerebrospinal fluid around your spinal cord during a lumbar puncture. An alternative way is to place a catheter which acts as a reservoir from which the drugs are ingested into the body.
Chemotherapy into the eye (intravitreal chemotherapy)
The drugs are directly injected in the eye. It is way simpler after the anaesthesia is given to patients but has several side effects on other organs of the body.
Topical eye drops of chemo are also given for cancers which are on the surface of the eye.
High-dose chemo followed by stem cell transplant
This method involves the storage of stem cells before chemotherapy. The blood-forming stem cells are taken from the patient’s body before the therapy so that they are not destroyed during the therapy. After the chemo has been given, they infuse the stem cells back into the body. These cells settle in the bone marrow, where they make new blood cells.
Other therapies for eye cancer treatment are
- Immuno-therapy drugs: They work by helping body’s own immune system and attack cancer cells. For example, pembrolizumab (Keytruda) and ipilimumab (Yervoy).
- Targeted drugs: They target only parts of the melanoma cells. For example, BRAF gene suffers mutation during skin melanomas but no impact on uveal melanomas. Still, studies are going on the target drugs as a potential treatment option for eye cancer.
- Monoclonal antibodies: They target cancer cell surface and helps fight the infection. For example, Rituximab (Rituxan) is an antibody attached to the substance called CD20, found in the surface of many lymphoma cells, and helps kill the cancer cells. Another example is a radioactive molecule known as Ibritumomab tiuxetan (Zevalin). Both these are used as chemo drugs.
- Cryotherapy: It can freeze the cancerous cells. Extreme cold destroys small retinoblastoma tumors. Cryotherapy may cause provisional swelling of the eye and eyelid. It is repeated several times.
- Thermotherapy: It mechanizes heat to destroy the cancer in the form of small tumors in certain locations.
Side effects of various eye cancer treatments
Side effects of eye cancer surgery
- It can sometimes lead to loss in some or entire vision
- Anesthesia can have some possible side effects such as infection, fatigue, pain, blood clot etc
- Removal of the eyeball can affect a person’s appearance which can be minimized to some extent by an artificial eye
Side effects of radiation therapy and laser therapy for eye cancer treatment
- Problems such as cataract, glaucoma, retinal detachment or bleeding in the eye arise after exposure to the radiations and laser. The intensity of radiations depends on the size and location of the tumor.
- Radiation therapy is directly linked to the brain and spinal cord and therefore, sometimes might lead to loss in memory, which gets worse with time.
- The following side effects are less common and can cause a loss of vision:
- Radiation retinopathy: Abnormal blood vessels are developed in the retina.
- Radiation optic neuropathy: Damage to the optic nerve.
- Neovascular glaucoma: The outflow of fluid is blocked with the development of new blood vessels which might be a painful condition.
- Loss of eyelashes and/or a dry eye: These side effects can occur with external-beam radiation therapy and proton-beam radiation therapy. The eye may need to be removed if the damage is significant.
Side effects of chemotherapy for eye cancer
- This technique hinders the quick phenomenon of cell division with the help of chemo drugs.
- These drugs have certain side effects depending on the type and dosage of the drug such as:
- Loss of hair
- Mouth sores
- Nausea, fatigue and vomiting
- Diarrhea and constipation
- Loss of appetite
- High chances of infection
- Easy bruising and bleeding
What happens after the treatment of eye cancer?
Completing the treatment can be both exciting and stressful because although the cancer is being killed but it can reoccur anytime in future. It is very uncertain as to when it will again recur and start building up. Regular follow-up checks are necessary which also allow keeping a track of the side effects, if they occur.
For eye cancer, regular checkups should be done every month after the treatment of both the eyes. Blood tests and imaging tests should be done for complete body because it clears the possible signs that cancer has not spread to other parts of the body. If there is any such sign to indicate that the eye cancer is re-occurring or has affected any other organ, the treatment can be started again when it is in a mild phase.
Coping with eye cancer (Living with eye cancer)
One major effect of eye cancer and its treatment is that a person suffers both mentally and physically which results in several other problems. Change in physical appearance extremely affects a person. Drugs also have side effects which cause many issues. The only way to manage these issues is to cope with the disease better with effective strategies and to stay positive.
How can having an eye cancer affect your emotional health?
It happens normally to most of the people who suffer with cancer. An emotional setback or anxiousness can make the patient feel negative. The person may feel weak. Thoughts of death and dying, concern of finance can be stressful. Managing career, friends and family can be difficult which affects the lifestyle at an extreme.
One can deal with it with complete positivity. Support of friends and family can be a major uplift. These days, online support groups, healthcare professionals and counselors can be a backup support system to the patient.
Lifestyle Changes after Having Eye Cancer
Adopting healthy habits
Keeping healthy eating habits is one big factor which affects any cancer. The consumption of tobacco and alcohol should be cut down to zero.
Positive thinking is one best way to reduce the risk of cancer to spread fast to other areas as it keeps one healthy and strong.
The sense of taste changes after the treatment which can be frustrating. The only way is to adopt a healthy lifestyle by various ways such as maintaining a healthy diet, adding variety to it, avoiding harmful foods, regular consultation with the doctors etc.
Rest, fatigue and exercise
Fatigue (extreme tiredness) is a common problem that affects cancer patients which can only be reduced by regular physical activity and staying active. Rest is also necessary because the body has undergone through a severe disease and its intensive treatment, and therefore needs time to recover.
Exercise is one best way to lower down the dullness and staying energetic. This surely keeps a person healthy both physically and emotionally.
- It keeps away fatigue and keeps the person feel light and energized.
- Exercise lowers the level of depression and anxiety.
- It improves the cardiovascular system of the body by keeping a person fit.
- It maintains a healthy body physically by keeping muscles fit and emotionally by keeping a person happy.
Watching for reoccurrence or remission of eye cancer and how the risk can be reduced
A remission is when there are no symptoms of eye cancer and it cannot be diagnosed. This may also be called having “no evidence of disease” or NED. It can be temporary or permanent.
Cancer recurs because small areas of cancer cells may remain undetected in the body. Regular checkups are to be done to check for the metastasis. Blood tests and imaging tests are necessary to determine the stage and type of cancer and should be done as routine checkup for patients who have already suffered with cancer.
Adopting a healthy lifestyle i.e. quit smoking, drinking or tobacco consumption to reduce the risk of reoccurrence of eye cancer.
Eye cancer treatment failure
Recovery from eye cancer is not always possible. The advance stage of cancer cannot be controlled and is incurable. All the treatments have failed at this stage and the cancer continues to grow. Even the best and newer treatments have failed to work. Clinical trials can sometime be effective in such cases but that is a very rare phenomenon.
The maximum life a patient is left at the terminal stage is of six months. It is a very stressful situation and therefore the patient is given a lot of care. These are the moments which are made to live completely because staying happy and hopeful is very important.