How Is Psoriasis Diagnosed and Treated?
- Updated on: Nov 22, 2024
- 6 min Read
By
- Published on Oct 3, 2019


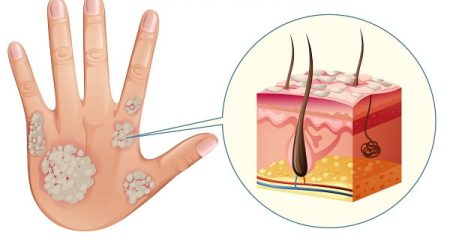
Psoriasis is a long-lasting chronic skin disorder, which is characterized by red, itchy and scaly patches all over the skin.
Diagnosis of psoriasis
Diagnosis of psoriasis is the process of identifying the nature of psoriasis (or its type) by carefully looking at the symptoms. Diagnosis of psoriasis is mainly straightforward. Psoriasis cannot be diagnosed by any blood tests or other procedures. There are two ways by which it is diagnosed:
Physical examination of skin and medical history
Your local dermatologist can easily diagnose the disease by doing a physical examination. By simply looking at the skin, scalp and nails, the doctor can tell the nature of the disease.
Medical history is also very important in its diagnosis. If any close relative of the patient has been diagnosed with the disease, there are fair chances of the patient to be diagnosed with it.
Since psoriasis can look like other skin infections such as eczema, it can be sometimes very difficult to diagnose the disease.
Skin Biopsy
- Process of diagnosis in which a small sample of affected tissue is taken after applying a local anesthetic, which is then examined under a microscope to make a definitive diagnosis.
- The method allows distinguishing it from other types of skin allergies and infections.
- Allows to determine the exact type of psoriasis
- Rule out other diseases
Once your diagnosis is complete, you need to see a dermatologist. A dermatologist is a specialist in the diagnosis and treatment of skin diseases like psoriasis and cellulitis. He/she can answer all your questions and offer insights on how to deal with psoriasis.
The patient must be honest with his/her dermatologist, and should clearly describe all the signs and effects of the disease to the doctor. This will be helpful in determining the impact psoriasis has on the life of the patient, both physically and emotionally.
Topics to discuss with your dermatologist include:
- Change in symptoms if any
- Any symptoms other than usual ones
- How psoriasis affects on the dressing
- How often the psoriasis flares up and in what manner
- How is current treatment going and are there any side effects
- Stress or embarrassment faced by the patient due to psoriasis
- Any joint pain the patient may have
- Other medical conditions
- Medications patient may be taking, including over-the-counter and herbal products
Treatment of Psoriasis
Psoriasis cannot be cured completely, still, there are some ways to ease the symptoms of psoriasis and make them less effective.
There are many ways and methods to deal with the disease. Some of the methods can even be applied together. If one treatment option doesn’t work, something else likely will.
Before treating the disease, the doctor will make a treatment plan based on:
- How severe the condition is
- How much the patient is willing to do and to what extent
- What treatments the patient has already used
- Whether the patient has any other medical conditions
Psoriasis treatment can be divided into three main types: topical treatments, light therapy and systemic medications. They can be used in combinations also.
Topical treatments
This treatment is used when the disorder is not severe; that is when the symptoms are mild to moderate.
These are cream-based medications that are applied to the affected parts of skin at regular intervals. Topical treatment is combined with oral medications or light therapy if the doctor feels that the disease is more severe. Topical psoriasis treatments include:
Topical corticosteroids
- These are most frequently prescribed medications
- Reduce inflammation and relieve itching
- Mild ointment is prescribed for sensitive areas, such as your face
- Strong ointment is suggested for smaller, less sensitive areas
- Can cause thinning of the skin if used for a long time
- May stop working after a particular time
- Work best as a short-term treatment during flares
Vitamin D analogues
- These are artificial forms of vitamin D
- Cream based medications like Calcipotriene
- Slow down skin cell growth
- Ideal for mild to moderate psoriasis
- May irritate skin
Topical retinoids
- Vitamin A derivatives
- May decrease inflammation
- May cause skin irritation
- May also increase sensitivity to sunlight, so sunscreen is advised while using the medication
Calcineurin inhibitors
- Reduce inflammation and plaque build-up
- Not good for the skin if used continuously for long time as they may cause skin cancer
- Helpful in areas of thin skin, such as around the eyes
Salicylic acid
- Increase shedding off dead skin cells and reduces scaling
- To be more effective on the affected area these are combined with other medications, such as topical corticosteroids and coal tar.
- Available as medicated shampoos and scalp solutions to treat scalp psoriasis
Coal tar
- Derived from coal
- Reduces scaling, itching and inflammation
- Irritate the skin
- Messy, stains clothing and bedding
- Has a strong odor
- Available as over-the-counter shampoos, creams and oils
- Not recommended for women who are pregnant or breastfeeding
Moisturizers
- Available as moisturizing creams
- Reduce itching, scaling and dryness
- Ointment base is usually more effective
- Should be used immediately after a bath or shower to lock in moisture
- Alone cannot heal psoriasis. They works well with other medications
Light therapy (phototherapy)
It involves treatment with light. It uses natural or artificial ultraviolet light.
- Sunlight can be used for the therapy
- Exposing the affected area in sunlight or artificial light can be considered
- It slows down skin cell turnover
- It reduces scaling and inflammation
- Daily exposures to small amounts of sunlight may improve psoriasis
- Intense sun exposure can make the situation even bad and thus damage the skin
UVB phototherapy
- Also called broadband UVB
- An artificial light source is used to inject controlled rays of UVB light
- Improves mild to moderate psoriasis symptoms
- Can be used to treat single patches, widespread psoriasis and psoriasis that resists topical treatments
- May cause redness, itching and dry skin. Using a moisturizer can be effective in dealing with these side effects.
Narrowband UVB phototherapy
- This is a newer type of psoriasis treatment
- In most cases, it is more effective than broadband UVB treatment
- It is usually given two or three times a week until the skin improves, and then few more weeks are required for maintenance
- It may cause more severe and longer lasting burns
Goeckerman therapy
- Combination of UVB treatment and coal tar treatment
- More effective because coal tar makes skin more receptive to UVB light
- Psoralen plus ultraviolet A (PUVA)
- Involves taking a light-sensitizing medicine like psoralen before exposure to UVA light. UVA light penetrates deeper into the skin and makes the skin more responsive.
- It is a more aggressive treatment
- It consistently improves skin
- Often used for more severe cases of psoriasis
- May cause nausea, headache, burning and itching for short term
- Dry, wrinkled skin, increased sensitivity to sun, and increased risk of skin cancer, are long term side effects
Excimer laser
- A form of light therapy
- Used for mild to moderate psoriasis
- Healthy skin is not at all affected
- Treats only the scaly skin
- A controlled beam of UVB light is directed to the psoriasis plaques
- Controls scaling and inflammation
- Lesser number of sessions are required than those in traditional phototherapy because more powerful UVB light is used in it
- May cause redness and blistering
Oral or injected medications
If other medications and treatments are not able to treat the condition effectively, the doctor may prescribe oral or injected drugs. It is also known as a systemic treatment.
The medications are used for short periods and may be changed eventually with other forms of treatment, because of severe side effects. Main medications used are:
Retinoids
- Related to vitamin A
- Helps in severe psoriasis that doesn’t respond to other therapies
- Lip inflammation and hair loss are the side effects
- Women must avoid pregnancy for at least three years after taking the medication because certain retinoids such as acitretin can cause severe birth defects
Methotrexate
- Taken orally
- Suppresses the speedy production of skin cells and reduces inflammation
- May also slow the progression of psoriatic arthritis in some people
- Works best in low doses but may cause upset stomach, loss of appetite and fatigue
- May cause severe liver damage and decrease the production of red and white blood cells and platelets when used for a longer span of time
Cyclosporine
- Suppresses the immune system
- Similar to methotrexate in effectiveness
- Can only be given for a short period
- Increases risk of infection and other health problems, including cancer
- Makes the person more susceptible to kidney problems and high blood pressure
- Higher dosages and long-term therapy can worsen the situation
Biologics
- Drugs that alter the immune system
- These are given by injection
- Used for people who have failed to respond to traditional therapy
- Used for people who have associated psoriatic arthritis
- Have strong effects on the immune system, and must be used very carefully
- May permit life-threatening infections
- May cause tuberculosis