How to Protect Yourself From Antibiotic Resistant Foodborne Illnesses?
- Updated on: Jun 29, 2024
- 4 min Read
- Published on Dec 1, 2020

Antibiotic resistance in foodborne microbes has become a major public health concern. Most of the foodborne illnesses are mild and get cured without treatment. Most of the foodborne illnesses can be treated with antibiotics. However, some foodborne bacteria have developed antibiotic resistance and are difficult to treat.
What Is Antibiotic-Resistant Foodborne Illness?
Antibiotic resistance refers to the ability of microbes to withstand the effect of antibiotics. Antibiotics are powerful drugs to fight against many bacterial illnesses in people. Bacteria usually become resistant to antibiotics when people take antibiotics unnecessarily without consulting a doctor.
Animal foods such as cattle, chicken, pork, and lamb are the major source of antibiotic-resistant bacteria infections and are responsible for developing foodborne illness in people. Some examples of antibiotic-resistant foodborne bacteria are Campylobacter, Salmonella, Escherichia coli, and Listeria monocytogenes. These bacterial infections are more likely to occur through animal food products.
Food producing animals are generally treated by various antibiotics to treat, control, and prevent infections. All these animals contain a large number of bacteria within their intestines. When such animals are given a high dosage of antibiotics, it results in antibiotic resistance within their digestive system. These antibiotic-resistant bacteria easily transmit from food-producing animals to humans. When humans consume such animal foods contaminated with antibiotic-resistant bacteria, it causes antibiotic foodborne illnesses.
Besides, these antibiotic-resistant bacteria can transmit from animal feces, fruits and vegetables are grown on the soil infected by these bacteria, and through the environment.
People can develop antibiotic-resistant foodborne illness in the following ways:
- Eating contaminated meat and poultry.
- Eating foods that have been contaminated with juices released from the raw meat due to its improper handling.
- Using equipment already contaminated with antibiotic-resistant bacteria through raw meat, such as chopping boards, knives, and other utensils.
- Coming in contact with the animal feces contaminated with antibiotic-resistant bacteria.
- Not maintaining good hand hygiene after preparing the raw meat.
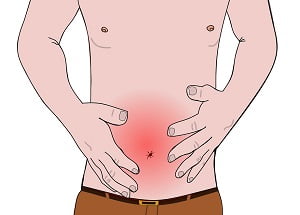
The symptoms associated with antibiotic-resistant foodborne illness are:
- Diarrhea
- Vomiting
- Nausea
- Fever
- Headache
- Abdominal cramps
- Weakness
Read People With Higher Risk of Food Poisoning
Read Risks of Raw Milk Food Poisoning
How to Protect Yourself From Antibiotic-Resistant Foodborne Illness?
Although the infections caused by antibiotic-resistant bacteria are difficult to treat, we can somehow prevent the spread of such infections to some extent. According to the Center for Disease Control (CDC), the following are some of the steps that can be followed to protect ourselves and our families from foodborne illness caused by antibiotic resistance:
- Do not take antibiotics without being prescribed by doctors.
- Take antibiotics in proper doses as recommended by the doctor.
- Cook your food at an appropriate temperature. A food thermometer can be used to check the temperature of the food.
- Watch your hands with soap and water before and after preparing the raw meat. Also, wash everything in contact with the raw meat, such as knives, chopping boards, kitchen surfaces, and other utensils.
- Keep raw meat and poultry items away from other foods to avoid cross-contamination.
- Use separate chopping boards for raw meat and other vegetables that need not be cooked before consuming, such as salads.
- Wash the raw meat thoroughly with warm water before cooking.
- Keep your refrigerator at a temperature of below 40?F and refrigerate foods within 2 hours of cooking in winters and within 1 hour if the outside temperature is above 90?F.
- Wash your hands properly with water and soap before touching the animals, their feces, etc.
- Keep your animal food items and vegetables separate from each other. Also, wash the vegetables thoroughly under running water before consumption.
- Avoid using unpasteurized milk and its products.
- Only consume pasteurized milk and milk products as pasteurization involves the killing of microbes via heating.
- Do not prepare food for others if you suffer from food poisoning symptoms like diarrhea and vomiting. Extra care should be taken when you have to prepare food for people with a weak immune system. Also, you should be careful when you are making food for older people and pregnant women as they are more susceptible to infections.
- During travel, prefer hot foods and drinks, especially the ones that are properly packed. Unpacked foods can increase your chances of food poisoning.
- Do not self-medicate, instead consult your doctor immediately if you recognize the symptoms of foodborne illness.
FAQs
What Antibiotics are Salmonella Resistant To?
Salmonella bacteria are found in food producing animals like ground beef, turkey, and chicken. These bacteria are resistant to antibiotics such as:
- Ampicillin
- Chloramphenicol
- Amoxicillin-clavulanic acid
- Sulfisoxazole
- Ceftiofur
- Tetracycline
- Ceftriaxone.
How Does Antibiotic Resistant Food Borne Illness Occur?
When animals are given a high amount of antibiotics, some bacteria that are present in their intestine become resistant to these antibiotics. These bacteria start to grow in their digestive system. These antibiotic resistance bacteria transmit to people when they eat the meat produced from these animals or other foods contaminated with the feces of these animals. This leads to antibiotic- resistant food borne illness among people.
What Are the Effects of Antibiotic Resistance?
Antibiotic resistance can affect any person at any stage of life. People who have a weak immune system are at high risk of getting an infection. Antibiotic resistance decreases a person’s ability fight against infections. This results in many symptoms such as frequent illness, more recovery time, and may also lead to death in some cases.
Can you Reverse Antibiotic Resistance?
Yes, antibiotic resistance can be reversed, but this process occurs very slowly. If you reduce the selective pressure that has been exerted due to the high amount of antibiotics, the bacterial population is likely to respond differently. They can potentially revert to a population of bacteria that responds to antibiotics.












1 Comment
There is perceptibly a bunch to realize about this. I feel you made certain good points in features also.