Neuroblastoma (Children’s Cancer): Causes, Signs, Symptoms, Risks, Diagnosis, Prevention, Treatment, Stages
- Updated on: Jul 8, 2024
- 16 min Read
- Published on Jan 30, 2020
What is neuroblastoma? Is neuroblastoma a type of cancer?
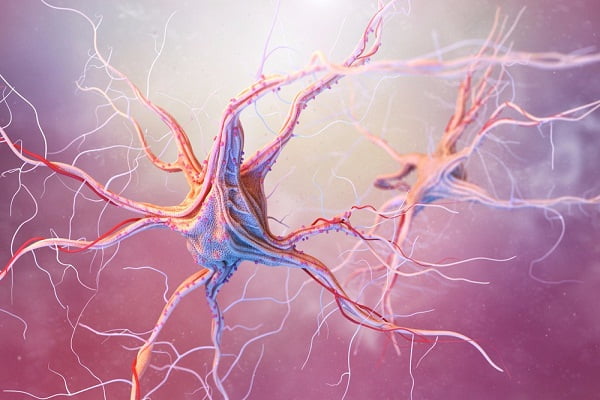
Neuroblastoma (also sometimes called Pediatric neuroblastoma) is a type of cancer that develops from immature nerve cells found in several areas of the body. These nerve cells are in their very early developmental stages, usually found in embryo or foetuses.
The word neuroblastoma consists of two terms where ‘neuro’ refers to nerves, and ‘blastoma’ refers to a cancer that affects immature or developing cells. These nerve cells are also known as neuroblasts which are capable of dividing and transforming into a fully functional neuron.
Neuroblastomas mainly affect infants and young children of age less than 5 years. Its occurrence in children older than 10 years of age is very rare.
Neuroblastoma most commonly arises in and around the adrenal glands situated above the kidneys, or the nerve tissues that are found alongside the spinal cord in the neck, chest, tummy and the pelvis. However, neuroblastoma can spread to other organs such as the bone marrow, bone, lymph nodes, liver and skin.
More: Adrenal gland cancer
More: Graphics, images, and photos for neuroblastoma
While some forms of neuroblastoma may go away on their own, others may require multiple treatments. Your child’s neuroblastoma treatment will depend on several factors including the type of neuroblastoma.
Is neuroblastoma a rare cancer? How common is neuroblastoma?
Neuroblastoma (Pediatric neuroblastoma) is a rare type of cancer that mostly affects the sympathetic nervous system (SNS) of babies and young children. SNS is the network of nerves that carries messages from your brain to the rest of your body.
There has been no change in the new cases of neuroblastoma diagnosed in the United States for many years. On an average, each year 700 new cases of neuroblastoma are diagnosed. There has been no change in this figure for many years and it has remained almost same. It is the third most common type of cancer in children and accounts for 6% of all childhood cancers in the United States. Neuroblastoma is usually found in children younger than 5 and most commonly in babies younger than 1 year old.
Pediatric neuroblastoma is diagnosed in children at an average age of about 1 to 2 years. In very rare cases, it is detected by ultrasound even before birth. Almost 90% of cases are diagnosed by age of 5 years.
For every 3 new cases diagnosed for neuroblastoma, in 2 cases, it has already spread to the lymph nodes or to other parts of the body.
Is neuroblastoma a cancer of the brain? Where does neuroblastoma originate from?
Neurobalstoma is a type of cancer which develops in nerve tissue outside of the central nervous system. The most common site of origin for this cancer is either the two adrenal glands present on the kidneys or in nerve tissues that run alongside the spinal cord, in the neck, chest, abdomen or pelvis. However, it can occur anywhere in your body.
Despite its confusing name, neuroblastoma is not a brain tumour. It is the most common extra cranial solid tumour found in children.
What causes neuroblastoma? Why do you get neuroblastoma?
The exact cause of pediatric neuroblastoma in children is unknown. To better understand it, you should know the difference between nueroblastoma and nuroblasts from which this type of cancer originally develops.
Neuroblasts are immature nerve cells found in unborn babies that a foetus makes as a part of its developmental process. When the foetus matures, normal neuroblasts eventually mature into nerve cells or the cells found in the centre of the adrenal gland also known as adrenal medulla cells. Sometimes, babies are born with small clusters of neuroblasts with them. If these cells do not mature and keep growing, it forms a mass known as tumour which ultimately becomes cancer. Neuroblastoma is the result of unchecked growth and improper maturity of these neuroblast cells.
Abnormal DNA inside the cells is believed to be the primary cause due to which some neuroblasts fail to mature and stop growing. DNA is the chemical that makes up our genes which instructs our cell function and behaviour.
Generally, neuroblasts get mature completely in the foetus by the time they are born, but sometimes babies are born with cluster of neuroblast cells, which eventually mature into nerve cells or simply die off or go on their own. However, in some cases, these cells fail to mature and do not stop dividing and growing. It becomes less likely that these cells will mature and more likely that they will grow into a cancer as children get older.
Can neuroblastoma be inherited?
It is very rare to inherit neuroblastoma from parents or even to inherit the gene changes which can cause neuroblastoma. There are some instances where neuroblastoma was found to be inherited because of genetic changes in some specific oncogene. However, most neuroblastomas are not caused by inherited DNA change rather they are the result of gene changes that happen early in the child’s development, often before birth. These changes are found only in a child’s cancer cells and can’t be passed on to his or her children.
What are the risk factors for neuroblastoma?
Lifestyle-related risk factors are not thought to play much of a role in childhood cancers, including neuroblastomas.
Exposures of environmental factors to the mother during pregnancy or in early childhood have no effect on increasing the chance of getting neuroblastoma.
Young age of children is a possible risk factor for neuroblastoma but even in this age group, it is rare. People over 10 years of age very rarely get neuroblastoma.
Children who have a family history of neuroblastoma may be more likely to develop the disease. Yet, the number of familial neuroblastoma cases is very small.
What are the signs and symptoms of neuroblastoma? What does neuroblastoma do to you?
The signs and symptoms of neuroblastoma largely depend on the location of the tumour, nearby tissues it’s affecting, size of the tumour, whether it has spread to other parts of the body, if the tumour cells secrete hormones.
Signs and symptoms of neuroblastoma present in belly or pelvis area
If the tumour has started in the abdominal or pelvic region, it may manifest following symptoms.
- Swallowing or presence of large lumps in the abdomen
- Children do not feel to eat leading to severe weight loss
- Older children may complain of feeling full
- Abdominal pain
- Changes in bowel movements such as diarrhoea and constipation
- Swelling in legs and scrotum due to blockage blood and lymph vessels supplying to these organs when the tumour presses on these organs
- Problems in urinating due to pressure of tumour on bladder and bowel
Symptoms of neuroblastoma in chest and neck
Neuroblastoma in these regions are often felt or seen as a hard and painless lump. Symptoms may include:
- Chest pain
- Back pain
- Wheezing
- Unexplained weight loss
- Changes to eyes such as drooping eyelids and unequal pupil size
- Lumps of tissue under skin
- Eyeballs that seem to protrude from the sockets (proptosis)
- Dark circles, similar to bruises, around the eyes
- Fever
- Bone pain
- Swelling in the face, neck, arms, and upper chest , sometimes with a bluish-red skin colour due to pressure from tumour on superior vena cava
- Coughing and trouble breathing or swallowing if the tumour presses on the windpipe
- Difficulty in moving arms and legs
Symptoms due to neuroblastoma that has spread to the other parts of the body
Neuroblastoma originating from anywhere in the body can spread to nearby or distant lymph nodes and make them swell. Swollen lymph nodes can be found as lump under the skin especially in the neck, above the collarbone, under the arm, or in the groin. You should note that enlarged lymph nodes can also be a sign of infection and not just a cancer. You should consult your doctor if your child is having enlarged lymph nodes in these areas of the body.
Neuroblastoma also spreads to the bones and can cause bone pain. Infants having neuroblastoma may not complain about it but a child who can talk may complain of bone pain. Due to this pain, your child may limp or refuse to walk. If neuroblastoma spreads to the bones in the spine, tumours here can press on the spinal cord and cause weakness, numbness, or paralysis in the arms or legs. This can cause pinching (compression) of nerves in your back.
Sometime, bumps under scalp are observed, if the neuroblastoma has spread to the other bones in the skull.
Nueroblastoma can also spread to the bone marrow. Bone marrow is the inner part of certain bones that makes blood cells. Spread of the cancer to the bone marrow can lead to shortages of blood cells that can result in tiredness, irritability, weakness, frequent infections, and excess bruising or bleeding from small cuts or scrapes.
A special form of neuroblastoma (stage 4S) which is found only during the first few months of life can spread to the liver and skin. In this case, a blue or purple bump that looks like small blueberries may be a sign of spread to the skin. An enlarged liver which can be felt as a mass on the right side of the belly is a sign of this condition.
Symptoms caused by hormones from the tumour
Sometimes, neuroblastoma cells may secrete certain chemicals or release hormones that can cause problems with tissues and organs in other parts of the body, even though the cancer has not spread to those tissues or organs called as paraneoplastic syndromes.
Symptoms manifested by paraneoplastic syndromes can include:
- Constant diarrhoea
- Fever
- High blood pressure (causing irritability)
- Rapid heartbeat
- Reddening (flushing) of the skin
- Sweating
Another rare paraneoplastic syndrome in people with neuroblastoma causes rapid eye movements and difficulty with coordination.
Diagnosis of neuroblastoma: How do you test for neuroblastoma?
Neuroblastomas are usually suspected when a child is brought to the doctor with one or more of the above mentioned signs and symptoms. After a physical examination of your ward, doctor may recommend various tests to confirm the diagnosis of a neuroblastoma.
Your doctor will seek a complete medical history if your child has any signs or symptoms that might be caused by a neuroblastoma. To know more about the symptoms your doctor might ask if there’s a family history of any type of cancer.
The doctor will perform a physical examination of your child for possible signs of a neuroblastoma and other health problems. During this examination, the doctor may be able to see or feel an abnormal mass or swelling in the body or may find a child has lumps or bumps under the skin or high blood pressure. Doctor will pay a close attention to posture and walking positions as neuroblastomas can sometimes grow close to the spinal cord and affect movement and strength in a child’s arms and legs.
Signs and symptoms such as enlarged lymph nodes and fever might be because of infection as well. To rule out any infection, doctor will look for other signs of infection at first.
If the history and physical examination is suggestive of neuroblastoma in a child, other tests will be ordered to confirm it. These diagnostic tests for neuroblastoma may include:
- Blood and urine test
- Imaging test
- Biopsy
Blood and urine catecholamine test for neuroblastoma
Blood and urine tests may indicate the cause of certain signs and symptoms your child is experiencing. Urine tests are used to check for elevated levels of certain chemicals that result from the neuroblastoma cells producing excess catecholamine.
Catecholamine is a category of chemicals which consists of hormones such as epinephrine, which enters the blood. These chemicals are then metabolized by the body into smaller pieces and eventually passed out of the body in the urine.
Majority of children suspected to have neuroblastoma will have increased levels of the chemical substances called vanillylmandelic acid (VMA), or homovanillic acid (HVA), in their urine. Both VMA and HVA are metabolites of the catecholamine produced by the tumour cells.
Determining the level of VMA and HVA in the urine can help confirm the diagnosis of neuroblastoma. Levels of these metabolites are also measured during and after the treatment. If the treatment is working, elevated levels of these chemicals fall down in urine and blood. These chemicals can also be used to monitor the tumour activity as these are produced by the tumour cells. High level of these chemicals indicates a very active tumour. Sometimes, these chemicals are also known as tumour markers for the neuroblastoma.
Imaging tests for neuroblastoma
Imaging tests are usually performed to take images of inside of the body by using X-rays, sound waves, magnetic fields or radioactive substances. These tests are done to help find if the suspicious area is cancerous, to determine how far the tumour has spread or if the treatment is working. Different imaging tests performed for the diagnosis of neuroblastoma are discussed below.
Ultrasound for diagnosing neuroblastoma
Ultrasound uses sound waves to generate a picture of organs or masses inside the body. Usually, it is the first test performed in small children if a tumour is suspected, because it is fairly quick and easy. It is capable of giving a good view of inside the abdomen and is most often used to look for tumours in the abdomen. It doesn’t use any kind of radiation.
The picture obtained with the help of an ultrasound is not as detailed as those with some other tests, therefore even if a tumour is found, CT or MRI scans might still be needed.
X-rays
Though x-ray images are not detailed enough to spot tumours but the doctor may order an x-ray of the chest or another part of the body as an early test if a child is having symptoms. But it’s not clear with X rays what might be causing these symptoms. It can be helpful in determining the spread of the tumour to the bone if the diagnosis of neuroblastoma has already been established. It is also recommended if your doctor suspects that the cancer has invaded the lungs.
Computed tomography (CT) scan for the diagnosis of neuroblastoma
A CT scan is used to obtain a 3-dimensional picture of the inside of the body taken from different angles with the help of x-rays. These pictures are then combined by a computer into a detailed, cross-sectional view that shows any abnormalities or tumours if present. It is also helpful in measuring the size of the tumour.
Typically, a special dye is injected into a patient’s vein before starting the procedure to get better details of the image. The special dye is also known as contrast medium.
Magnetic resonance imaging (MRI) scan for neuroblastoma diagnosis
MRI is used to obtain images of the soft tissues inside of the body. This technique is more efficient in spotting the tumours of the spinal cord. This technique of diagnosis uses magnetic fields to produce detailed images of the soft tissues of the body so there is no involvement of any kind of radiations.
It takes more time than CT scans, often up to an hour. Your child will be required to lie in the narrow tube of the machine for a longer time. There is a loud buzzing and clicking sound which comes out of the machine during its operation which may be disturbing for the lying child in the machine. For this reason, children are often given medicine prior to the test to help keep them calm or even asleep during the test.
MIBG scan
This test uses a chemical known as meta-iodobenzylguanidine (MIBG) which contains a small amount of radioactive iodine. MIBG is chemically similar to a hormone norepinephrine produced by our sympathetic nervous system. It is helpful in spotting neuroblastoma of bone, bone marrow and other parts of the body. This is injected into the patient’s body via vein and it is able to attach to the neuroblastoma anywhere in the body. After several hours or days, body is scanned with a special visualizing camera for the areas showing any radioactivity.
Many doctors perform this test as a standard measure to diagnose nueroblastoma in children. In some cases, a higher dose of this chemical is even used to treat the neuroblastoma.
Positron emission tomography (PET) scan
For PET scan, a small amount of a radioactive material is injected into a patient’s body. This radioactive material is used by tissues having high energy requirement. Since tumours tend to require high energy input, more of radioactive substance is taken up by the tumour, and then a scanner is used to detect this substance and produce an image. This test is used for the diagnostic purpose of neuroblastoma when that tumour fails to take up MIBG.
Biopsy for neuroblastoma diagnosis
Biopsy is thought to be the definitive diagnostic test of any type of cancer including neuroblastoma where tumour cells are examined under a microscope.
It can be performed as a standalone procedure to take out some of the tumour tissues outside the body and then subjected to microscopic examination and evaluation. It is called as closed or needle biopsy.
Other kind of biopsy is open or surgical biopsy which is performed along with the surgical treatment of the tumour. Here the whole tumour is taken out of the body and a small sample of tissue is taken and forwarded to a laboratory for the microscopic examination by a pathologist.
Biopsy can also be helpful in the grading of tumours of the nueroblastoma. In adults, biopsy is generally performed under a local anaesthesia but in children, it is preferred to use general anaesthesia before the test.
Bone marrow aspiration and biopsy for neuroblastoma
Neuroblastoma can often spread to the bone marrow which is the inner soft part of the bones. If the diagnosis of neuroblastoma has already been established by urine test of catecholamine or other tests, these tests are performed to assess the extent of tumour spread.
Bone marrow aspiration and bone marrow biopsy are two different procedures but both are generally performed at the same time.
Bone marrow consists of both a solid and a liquid part. In bone marrow aspiration, a sample of fluid part of bone marrow is taken out with the help of a needle while in a bone marrow biopsy, there is a removal of a small amount of solid tissue using a needle. These both samples are then analyzed under a microscope by a pathologist.
Both of these procedures are extremely painful since they are performed at the pelvic bone, which is located in the lower back by the hip. Generally, this test is performed under a local anaesthesia. But often other medicines are also given to children to reduce pain from the procedure.
Neuroblastoma Staging: What are the stages of neuroblastoma?
Staging of neuroblastoma is done to describe the cancer state, its location, if it has spread and affecting other parts of the body. Knowledge of stage of the cancer helps a doctor to choose best possible treatment for an individual case of the neuroblastoma.
There are mainly two types of systems used to assign a stage to neuroblastoma. These are described below.
International Neuroblastoma Staging System Committee (INSS) system
This system is based on the result of surgery to remove the tumour. According to this system neuroblastoma has 4 main stages with some sub-stages which are briefly described below.
Stage 1 neuroblastoma
In this stage, it is possible to remove the tumour completely with the help of surgery. Lymph nodes removed during surgery which are attached to the tumour may or may not contain cancer, but other nearby lymph nodes do not contain cancer.
Stage 2A neuroblastoma
The tumour is confined only in the area where it started and cannot be completely removed during surgery. Lymph nodes nearby the tumour do not contain cancer.
Stage 2B neuroblastoma
The tumour is confined only in the area where it started and its complete surgical removal is not always possible. This may or may not be possible. However, nearby lymph nodes do contain cancer.
Stage 3 neuroblastoma
The tumour has spread to the regional lymph nodes or other areas near the tumour but not to the other parts of the body. Tumour in this stage cannot be removed with surgery.
Stage 4 neuroblastoma
The original tumour has spread to lymph nodes in other parts of the body also known as distant lymph nodes, liver, skin, bones, bone marrow, and/or other organs, except for those listed in stage 4S.
Stage 4S neuroblastoma
This is also known as special neuroblastoma. Here the original tumour is confined only in the location where it started and the spread of the tumour is exclusive to the skin, liver, and/or bone marrow, in infants younger than one on the same side of tumour of the body where tumour is located.
The spread of this type of cancer to bone marrow is minimal. Sometimes, neuroblastoma at this stage goes away on its own and often doesn’t require any treatment.
International Neuroblastoma Risk Group Staging System (INRGSS)
INRGSS system of staging for neuroblastoma does not use the results of surgery to define the stage rather it lets doctors determine a stage before surgery, based on the results of imaging tests as well as other exams and biopsies. The stage can then be used to predict how much of it can be removed with surgery.
The INRGSS uses image-defined risk factors (IDRFs), which govern the assigning of stage under this system. IDRFs are the factors seen on imaging tests that explains either the tumour will be harder to remove or relatively easy. These IDRFs include things like the tumour invading into a nearby vital organ or growing around important blood vessels.
International Neuroblastoma Risk Group Staging System categorises neuroblastomas in 4 stages, which include:
Stage L1 neuroblastoma
The tumour is confined in the location where it started and has no IDRFs after various imaging tests such as MRI or CT.
Stage L2 neuroblastoma
Here IDRFs are found on imaging tests but the tumour has not spread beyond the area where it started and to the nearby tissue.
Stage M neuroblastoma
The tumour has spread to various parts of the body except the location described in stage MS.
Stage MS neuroblastoma
The tumour has spread to only the skin, liver and there is very little involvement of the bone marrow in patients younger than 18 months.
What are the risk groups for neuroblastoma?
For some cases of neuroblastoma, surgery alone is a cure while for some others surgery along with chemotherapy is a cure option. However, some children have very aggressive form of neuroblastoma that is difficult to treat. In these cases, the doctor can predict the probability of treatment success, or if the cancer can relapse or come back after the treatment by using a combination of factors.
A combination of factors such as clinical, pathologic and genetic markers is employed in INRG system of classification to predict the tumour growth and to understand how well will it respond to the treatment. These markers are used to define risk groups of neuroblastoma and can be classified into 4 categories of risk groups which include:
- Very low-risk group
- Low-risk group
- Intermediate-risk group
- High-risk group
Various factors which are used to categorise the risk group in INRG classification system are the following.
- The stage of the disease according to the INRG staging system
- Age at the time of diagnosis
- Histological category, such as maturing ganglioneuroma versus ganglioneuroblastoma, intermixed versus ganglioneuroblastoma or nodular versus neuroblastoma
- Grade or how cells of the tumour are differentiated
- Tumour cell ploidy, which is the DNA content of tumour cells
- MYCN gene status
- Chromosome 11q status
Treatment of neuroblastoma: Can neuroblastoma be treated?
Treatment for neuroblastoma in children depends on various factors which include the risk group of the cancer, the age of patient, stage of the cancer, type of cells involved in the cancer and whether there is any abnormality in the chromosomes and genes.
The doctor will use the information to select the most suitable treatment plan for an individual case. Based on the risk category, the doctor may choose a treatment or combination of treatments for neuroblastoma. Different treatment options for neuroblastoma include:
- Surgery
- Chemotherapy
- Radiation therapy
- Stem cell transplant
- Immunotherapy
- Retinoid therapy
Surgery for neuroblastoma
In a surgical treatment for neuroblastoma, the doctor removes the tumour and some surrounding healthy tissues. Surgery can be used to remove the whole tumour if it has not spread to other parts of the body. But, most of the time, a neuroblastoma is diagnosed only after it has spread to other body parts. If it has already spread, the doctor removes as much of the tumour as possible during the surgery.
Complete removal of the tumour largely depends on the tumour location and its size. If the tumour is attached to nearby vital organs such as lungs and spinal cord, its surgical removal becomes risky.
Surgeons may try to remove as much of the tumour as possible in case of intermediate-risk and high-risk neuroblastoma. To kill the remaining cancer cells, either chemotherapy or radiation therapy can be used.
Chemotherapy for neuroblastoma
In a chemotherapy procedure, anti-cancer drugs are used to kill the cancer cells. Usually, these drugs are administered orally and can be injected into the body via veins in some cases. However, there are side effects associated with chemotherapy which are manifested when it damages the healthy and fast growing cells such as cells in the hair follicles and in the gastrointestinal system.
Various chemotherapy drugs are used in combination for children with intermediate-risk neuroblastoma, often before a surgery to improve the chances that the entire tumour can be removed during the operation.
In high risk neuroblastoma cases, usually, a high dose of chemotherapy drug is required to either shrink the tumour or to kill any cancer cells that have spread elsewhere in the body. Chemotherapy is usually used before bone marrow stem cell transplant and surgery.
Following drugs are used in chemotherapy for children with intermediate-risk neuroblastoma.
- Carboplatin
- Cyclophosphamide
- Doxorubicin
- Etoposide
Drugs which are often used in children with a high risk neuroblastoma are.
- Busulfan
- Carboplatin
- Cisplatin
- Cyclophosphamide
- Cytokines
- Dinutuximab
- Doxorubicin
- Etoposide
- Ifosfamide
- Isotretinoin
- Melphalan
- Thiotepa
- Topotecan
- Vincristine
Side effects of chemotherapy include fatigue, risk of infection, nausea and vomiting, hair loss, loss of appetite, and diarrhoea. Once the treatment is finished, these side effects usually go away. The category and dose of the drug given and the duration for which a child receives the drug usually determines the severity of side effects.
Radiation therapy for neuroblastoma
Radiation therapy uses high-energy x-rays or other particles to kill and destroy the cancer cells. When the radiation is directed to the tumour from outside of the body with the help of a machine, it is known as external-beam radiation therapy. It is the most common form of radiation therapy used.
Radiation therapy is used for children with a low risk or intermediate risk neuroblastoma if the surgery or chemotherapy is not responding well. It can also be used in high risk neuroblastoma cases after the surgery and chemotherapy to prevent the recurrence of cancer.
It also has some side effects which may include fatigue, mild skin reactions, upset stomach, and loose bowel movements. Many of these side effects go away on their own once the treatment is complete.
Stem cell transplant for neuroblastoma
A stem cell transplant is a medical practice where a non-functional or diseased bone marrow is replaced by hematopoietic stem cells. Hematopoietic stem cells are highly specialized blood-forming cells found both in the blood stream and in the bone marrow.
It is commonly known as a stem cell transplant, rather than a bone marrow transplant because it is the blood stem cells that are typically transplanted, and not the actual bone marrow tissue.
Stem cell transplant is usually employed in children with high-risk neuroblastoma. They may receive a transplant using their own blood stem cells known as autologous stem cell transplant.
Immunotherapy for neuroblastoma
Immunotherapy uses drug agents to strengthen your immune system to fight with the cancer cells. Usually, children with high risk neuroblastoma or children who go under stem cell transplant are administered immunotherapy drugs which stimulate the immune system to kill cancerous cells.
Retinoid therapy for neuroblastoma
Retinoids are chemical substances related to vitamin A. They are believed to help some cancer cell












