Non-Celiac Gluten Sensitivity: A Comprehensive Guide
- Updated on: Mar 2, 2024
- 3 min Read
- Published on Mar 2, 2024

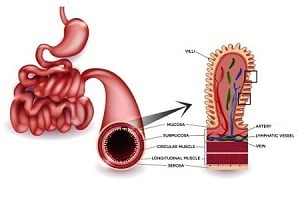
In recent years, the spotlight has increasingly focused on gluten and its effects on health, leading to a surge in gluten-free diets. While celiac disease has been well-documented, there’s growing awareness of a condition known as non-celiac gluten sensitivity (NCGS). NCGS presents a conundrum in the medical community, characterized by symptoms similar to those of celiac disease but without the autoimmune response or damage to the small intestine. This article delves into what NCGS is, its symptoms, diagnosis, management, and the current state of research.
Understanding Non-Celiac Gluten Sensitivity
Non-celiac gluten sensitivity is a condition wherein individuals experience symptoms related to gluten ingestion, in the absence of celiac disease or wheat allergy. Unlike celiac disease, NCGS does not have specific biomarkers, making it challenging to diagnose. It’s estimated that a significant portion of the population could be experiencing NCGS, though exact numbers are hard to pinpoint due to its nebulous nature.
Symptoms of NCGS
The symptoms of NCGS are diverse and can affect multiple systems in the body. Gastrointestinal symptoms may include abdominal pain, bloating, diarrhea, or constipation. However, NCGS can also manifest in non-gastrointestinal symptoms such as headache, “brain fog“, fatigue, joint and muscle pain, depression, and skin rashes. These symptoms typically appear after consuming gluten and improve or resolve upon adopting a gluten-free diet.
Diagnosis Challenges
The diagnosis of NCGS is complex and primarily exclusionary. Currently, there are no definitive tests for NCGS, so the diagnosis is made by ruling out celiac disease, wheat allergy, and other gastrointestinal disorders. This process often involves celiac disease serology tests, endoscopic biopsies, and wheat allergy tests. If these conditions are excluded and symptoms persist, a healthcare provider may suggest a gluten-elimination diet followed by a controlled gluten challenge to observe any symptomatic changes.
Management and Treatment
The primary treatment for NCGS is a gluten-free diet. Removing gluten from the diet has been shown to alleviate symptoms in individuals with NCGS significantly. However, due to the restrictive nature of the diet and potential nutritional deficiencies, it’s recommended to undertake this dietary change under the guidance of a healthcare professional or a registered dietitian.
The Gluten-Free Diet: Benefits and Considerations
Adopting a gluten-free diet can dramatically improve the quality of life for someone with NCGS. However, it’s important to approach this diet carefully to ensure it is balanced and nutritionally adequate. Gluten-free does not inherently mean healthier, as many gluten-free products are high in sugars and fats. Individuals should focus on a diet rich in fruits, vegetables, lean proteins, and gluten-free grains like rice, quinoa, and buckwheat.
Current Research and Future Directions
Research into NCGS is ongoing, with scientists striving to understand its pathophysiology better and to identify potential biomarkers for diagnosis. Some studies suggest that other components in wheat and gluten-containing grains, such as fructans (a type of FODMAP), may contribute to symptoms attributed to NCGS. This has led to a broader consideration of a low-FODMAP diet in managing symptoms for some individuals.
Future research aims to clarify the condition’s underlying mechanisms, improve diagnostic methods, and explore the long-term effects of a gluten-free diet on nutritional status and overall health. There’s also interest in understanding the role of the microbiome in NCGS and whether interventions targeting gut bacteria could alleviate symptoms.
Living with NCGS
Living with NCGS requires a significant lifestyle change, primarily through diet modification. However, with the increasing availability of gluten-free products and a growing public awareness of gluten-related disorders, it’s becoming easier to manage the condition. Support from healthcare providers, nutrition experts, and patient advocacy groups can provide valuable information and emotional support.
Final Thoughts
Non-celiac gluten sensitivity is a condition that poses diagnostic challenges due to its overlapping symptoms with other gluten-related disorders. While the path to understanding NCGS is fraught with complexities, adopting a gluten-free diet remains the cornerstone of managing symptoms. As research continues to unfold, there is hope for more precise diagnostic tools and targeted therapies. For now, awareness, education, and a collaborative approach to care are key to improving the lives of those affected by NCGS.
In navigating NCGS, it’s crucial to remember that each individual’s experience is unique. A personalized approach to diet and symptom management, guided by professionals, can help in effectively controlling this perplexing condition. With continued research and a growing understanding of gluten’s effects on the body, the future holds promise for those grappling with the challenges of non-celiac gluten sensitivity.