Overview of Psoriasis and Its Types
- Updated on: Jun 26, 2024
- 5 min Read
By
- Published on Oct 3, 2019

What is Psoriasis?
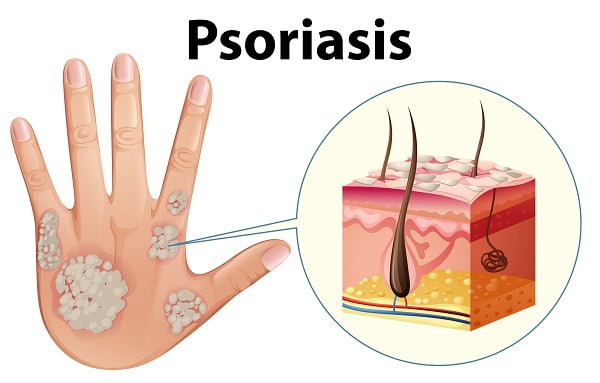
Psoriasis is a type of inflammatory skin disease in which the person affected suffers from skin redness and irritation. People affected with psoriasis have thick red scaling plagues of itchy skin.
Psoriasis is a common skin condition that speeds up the life cycle of skin cells. It causes cells to build up fast on the surface of the skin. These extra skin cells may form scales and red patches that are itchy and can sometimes be painful.
How Does Psoriasis Develop?
Generally, our skin cells grow deep in the skin and then rise to the surface about once a month. If you have psoriasis, this process takes place too fast. Dead skin cells build up on your skin’s surface. In most people, rashes are limited to only a few patches of the skin. In severe cases, it can cover large areas of your body too.
Psoriasis starts as small red bumps that grow in size, on top of which scale forms. These scales shed easily, but scales below them stick together. In addition, if these scales are scratched, the lower scales may tear away from the skin, which can cause bleeding.
Read more about signs and symptoms of psoriasis.
As the rash grows larger, “plaque” lesions can form. The rash usually can appear anywhere but mainly it affects the following areas of your body:
- Scalp
- Elbow
- Knees
- Lower back and genitals
- Finger nails
Psoriasis usually begins in early adulthood but it can start later in life. We can say it most commonly begins between ages 15 and 35.
The rash does not heal completely. It can come back anytime throughout a person’s life.
Is Psoriasis Contagious?
Psoriasis is a non-contagious disease and so it does not spread from one person to another. But it seems to pass down through families.
Doctors think it may be an autoimmune condition. This occurs when the immune system mistakenly attacks and destroys healthy body tissue.
Prevalence of Psoriasis
Psoriasis affects 1% to 3% of the world’s population. Environmental causes can trigger a psoriasis flare in people who have psoriasis. The good news is that avoiding these triggers can cut down on the number or severity of the flares. However, some of them are hard to avoid.
Triggers of Psoriasis Attack
Following are the few factors that may trigger an attack of psoriasis or make the condition even worse which actually is harder to treat:
- Bacteria or viral infections, including sore throat and respiratory infections such as common cold and viral
- Dry air or dry skin injury to the skin, including cuts, burns, and insect bites such as mosquito bite or wasp bite
- Some medicines such as anti-malaria drugs, beta-blockers
- Low levels of calcium
- Stress
- Too little sunlight
- Too much sunlight (sunburn)
- Alcohol consumption
Read more about causes of psoriasis.
People who have a weak immune system can be very easily affected by psoriasis and that too very badly. This may be due to following:
- Cancer chemotherapy
- AIDS
- Autoimmune disorders (such as rheumatoid arthritis)
Some people with psoriasis may also have arthritis (psoriatic arthritis).
Types of Psoriasis
Psoriasis is termed as a complicated disease because there are several different types of psoriasis. A person with psoriasis can have one or more of them at the same time, and the type of psoriasis may change throughout the person’s lifetime.
The area of skin involved may vary with the type of psoriasis you may have. Psoriasis patches can range from a few small spots of scaling similar to dandruff to major patches that cover large areas of your body.
Most types of psoriasis progress through cycles. This means there happens flaring for a few weeks or months, then subsiding for a time or even going into complete remission. The types of psoriasis are given here:
Plaque psoriasis
It is the most common form of psoriasis. Plaque psoriasis causes dry, red skin lesions (plaques) covered with silvery scales.
The plaques might be itchy or painful and these may be a few or many. They can occur anywhere on your body on the extensor surfaces of the knees, elbows, scalp, and trunk, including your genitals and the soft tissue inside your mouth.
The scale may be scraped away to reveal inflamed skin beneath. About 90% of all psoriasis is plaque psoriasis. This uncomfortable condition is slightly more common in men.
The plaques get bigger until they reach a certain size. They may not then change for months or several years.
Nail psoriasis
Psoriasis can affect your fingernails and toenails, causing pits to form on the nails. This often becomes thickened and yellowish. It is considered the most common nail finding, abnormal nail growth and discoloration.
Psoriatic nails might loosen and separate from the nail bed, known as onycholysis, due to the parakeratosis of the distal nail bed.
Severe cases may cause the nail to crumble. Exocytosis of leukocytes beneath the nail plate, cause oil spots and these are considered the most specific nail finding in psoriasis.
Psoriatic nails may not be distinguished from fungal nail. At the same time, they may be more prone to developing onychomycosis because of the nail separation.
Scalp Psoriasis
Scalp is the most common place for people with psoriasis to get a rash. Scalp psoriasis affects approximately 50% of patients. Some people may only have a small patch with some scaling, generally on the back of the head or your upper neck. Other people might have a raised, reddish rash that may cover their entire scalp.
Many individuals with scalp psoriasis mistakenly believe they have seborrheic dermatitis instead. While the former condition usually looks powdery and casts a silvery-looking sheen, the latter typically appears oily and yellowish.
With proper diagnosis and medication, healthcare professionals can treat psoriasis. Read about treatment of psoriasis.
Guttate psoriasis
This type primarily affects young adults and children. It is found in less than 2 percent of psoriasis cases.
It generally occurs one to three weeks after a viral or bacterial (generally streptococcus) respiratory infection. It is characterized by pink droplets (1 to 10 mm in diameter) on trunk, arms, legs and scalp, covered by fine scales.
The word “guttate” comes from the Latin word for drop, “gutta.” The flakes are covered by a fine scale and aren’t as thick as typical plaques are. You may have a single outbreak that goes away quickly on its own, or you may have repeated episodes.
Inverse psoriasis
Inverse psoriasis, also referred to as intertriginous psoriasis, is an unusual type of psoriasis that occurs in skin folds located in the armpits, in the groin, under the breasts and around the genitals.
Inverse psoriasis causes smooth patches of red, inflamed lesions without scaling due to the moist nature of the area where this type of psoriasis is located, that worsens with friction and sweating.
Fungal infections may trigger this type of psoriasis. This can make inverse psoriasis look like other skin conditions.
Pustular psoriasis
Pustular psoriasis (also known as von Zumbusch psoriasis) is a rare, sometimes fatal form of psoriasis. This type of psoriasis can occur on your hands, feet or fingertips either in smaller sections or wide-spreadly.
It generally develops quickly, with pus-filled blisters appearing just hours after your skin becomes red and tender. The blisters may come and go frequently. Despite its appearance, it is not contagious.
Generalized pustular psoriasis can also cause fever, chills, severe itching, diarrhea, dehydration, increased heart rate and other serious symptoms. They frequently require hospitalization as a result.
Erythrodermic Psoriasis
It is the least common type of psoriasis. Erythrodermic psoriasis can cover your entire body with a red, peeling kind of rash that can cause too much of itching or burning.
Fever, chills, and dehydration may follow it. Patients with severe pain may require hospital admission. Older patients with erythrodermic psoriasis may experience cardiac instability and hypotension due to massive vascular shunting in the skin.
Psoriatic arthritis
It affects approximately 10-30% of those with skin symptoms. It usually appears in hands and feet and, occasionally in large joints.
In addition to inflamed, scaly skin, psoriatic arthritis causes swollen, painful joints that are typical of arthritis. Sometimes the joint symptoms are the first or only manifestation of psoriasis.
Although this type of psoriasis is not as severe as other forms of arthritis, it can cause stiffness in the joints. This in turn can lead to progressive joint damage that in the most serious cases may lead to permanent deformity.












