Spinal Stenosis (Canal Stenosis): Causes, Signs, Symptoms, Risks, Diagnosis, Treatment
- Updated on: Jul 12, 2024
- 10 min Read
- Published on Apr 20, 2019
 Spinal stenosis – Definition and Overview
Spinal stenosis – Definition and Overview
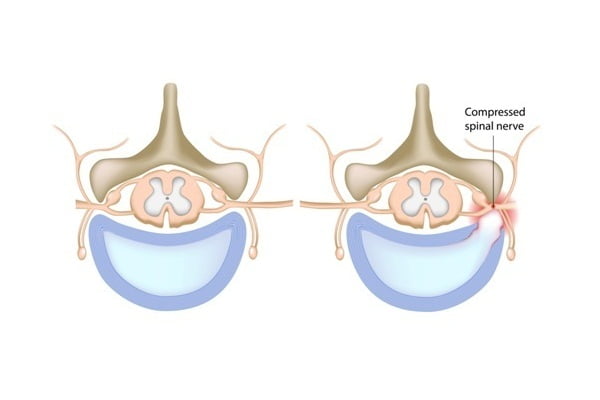
Spinal stenosis is the abnormal narrowing of spaces within the spinal canal (spine or neural foramen). This puts pressure on the nerves or on the spinal cord (or the roots) that travel through the spine. This narrowing limits the amount of space available for the spinal cord and nerves. As a result, the spinal cord is compressed by this narrowing of spaces within the spinal canal. With an increase in severity of the spinal stenosis, there is increased compression or squeezing of the spinal cord and its nerves. The condition is also referred to as canal stenosis.
The spinal cord passes from the brain through the spinal canal and travels down the back. The nerves of the spinal cord run between vertebrae of the neck and the lower back carrying signals from the brain. This controls the movements of arms and legs. The spinal canal is the cavity formed by the central openings of successively placed bones (vertebrae) and stacked on top of each other. The canal is attached to the head at the top and to the pelvis at the bottom.
Spinal refers to “spine” and the term “stenosis” comes from a greek word which means “choking” or “narrowing or constricting space”. Stenosis, in medical terminology, is used to describe the condition where a normal-size opening becomes narrow.
Other names for spinal stenosis are pseudo-claudication, central spinal stenosis and foraminal spinal stenosis.
Spinal stenosis can affect the cervical (neck), thoracic (chest), or lumbar (lower back) spines. But the most affected areas due to spinal stenosis are lower back and neck.
More: Graphics, images, photos of spinal stenosis
Types of spinal stenosis (narrowing of the spine)
Depending upon the area where the pain begins, spinal stenosis is differentiated into the following types:
- Cervical spinal stenosis: Cervical spinal stenosis occurs in the upper part of the spinal canal i.e. the neck.
- Lumbar spinal stenosis: Lumbar spinal stenosis occurs in the part of the lower back i.e. the lumbar spine.
- Central canal stenosis: The middle part in the thoracic spine of the midback is where central canal stenosis occurs.
Spinal stenosis occurs in about only 10% of the population and most commonly in people over the age of 50. Both the genders are affected equally.
The first modern description of the spinal stenosis came out in 1803 by Antoine Portal; although evidences of the condition were first noted earlier in Ancient Egypt.
Signs and symptoms of spinal stenosis
The symptoms of spinal stenosis gradually progress with time, as the spinal nerves get more compressed. The symptoms of spinal stenosis occur very slowly.
Some of the most common signs and symptoms of spinal stenosis include:
- Weakness and cramping in legs, shoulders or arms
- Pain in the lower back and neck especially with discomfort in standing or walking
- Numbness in knees, legs or buttocks
- Balancing problems
- Foot problems
- Local and traveling pain throughout the nerves in the back
- Burning sensation and tingling
- Loss of fine motor skills
Symptoms specifically for the pain in the neck (cervical spine)
- Numbness or tingling in hands, arms, feet or legs
- Weakness in hand, arms, feet or legs
- Problems while walking and balancing
- Neck pain
- Bowel or Bladder dysfunction (urinary urgency and incontinence)
Symptoms specifically for the pain in the lower back (lumbar spine)
- Numbness or tingling in feet or legs
- Weakness in a feet or legs
- Pain or cramping in one or both legs while standing for longer time periods or while walking.
- Pain in back
Risk factors which can lead to spinal stenosis
Age
Due to natural aging process, narrowing of spinal canal can occur as a result of several conditions. With increasing age, the ligaments in the spine become thicker, bone spurs or bony edges grow on the vertebrae of the spine, discs in between vertebrae may deteriorate and misalign along the spine. All of these aging-related occurrences can lead to thinning of the spinal canal which puts pressure on the nerve roots or on the spinal cord.
Breaking down of facet joints or the formation of cysts on the facet joints also result in compression of the spinal sac of nerves (thecal sac). This also occurs due to aging.
Congenital
In some cases, the spinal canal is too small at birth which most often leads to structural deformities. These deformities of the vertebrae may cause narrowing of the spinal canal.
Arthiritis and spondylolisthesis
The forward or anterior displacement of a vertebra over another vertebra inferior to it (or the sacrum) leads to the instability of spine. This is known as spondylolisthesis.
Osteoarthritis and rheumatoid arthritis can also cause spinal problems.
Trauma
Trauma or injury to the spine can cause vertebrae fractures or dislocations, which in turn can cause damage to the spine canal. Sometimes, accidents can also cause burst fractures that can restrict the space within the spinal canal. Narrowing of the spinal canal also increases the risk of acute spinal cord injury.
Tumors
Irregular or unexpected growth of soft tissue within or around the spinal canal can cause swelling or inflammation. This creates a pressure on the nerves (on the sac of nerves) or on the spinal cord.
Causes of spinal stenosis
The spine runs from the neck to the lower back. The backbone forms the spinal canal whose primary function is to protect the spinal cord (nerves).
Degenerative conditions such as osteoarthritis or degenerative spondylolisthesis are the main causes of spinal stenosis. Other causes of spinal stenosis may include rheumatoid arthritis, spinal tumors, trauma, Paget’s disease of the bone, scoliosis, genetic conditions such as achondroplasia, etc.
Other causes which lead to the narrowing of the spinal canal (spinal stenosis) are:
- Over or excessive growth of bone: Any damage of the spinal bones due to osteoarthritis can initiate the formation of bone spurs in the spinal canal. Paget’s disease is a bone disease that usually affects adults and can cause excessive growth of bones in the spine.
- Herniated disks: The shock absorbers (like cushions) between the vertebrae tend to dry out with increasing age. The cushioned material escapes out from the cracks (in a disk’s exterior) which create a pressure on the spinal cord or nerves causing discomfort.
- Thickened ligaments: The tough cords or the ligaments help in holding the bones of the spine together. These ligaments can become stiff and thickened over time. The thickened ligaments then bulge into the spinal canal in some cases causing irritation and pain.
- Tumors: Sometimes, uncommon (abnormal) growths can occur inside the spinal cord, within the membranes that cover the spinal cord or in spaces between the spinal cord and vertebrae. These uncommon growths can be identified by spine imaging with an MRI or a CT.
- Spinal injuries: Any dislocation or fracture in one or more vertebrae due to any mishap such as an accident or a trauma can lead to spinal injuries. Bone displacement (due to the spinal fracture) may damage the contents of the spinal canal. After back-surgery, any swelling in the nearby tissues can also put pressure on the spinal cord or nerves.
- Other factors that cause spinal stenosis: Certain conditions such as Bone spurs, Bulging disc or Spondylolisthesis can also result in spinal stenosis.
Diagnosis of spinal stenosis
The evaluation of spine is necessary for the diagnosis of spinal stenosis.
Medical history and physical examination
A physical examination is conducted to test the muscle strength, reflexes, sensation, balance, and circulation which help in determining the signs and symptoms of spinal stenosis. Specific locations where the nerve compressions might occur can also be detected through physical examination of spine.
Medical history is an important aspect during the diagnosis of spinal stenosis as it defines the symptoms, possible causes for spinal stenosis, and other possible causes of back pain.
Imaging tests for spinal stenosis
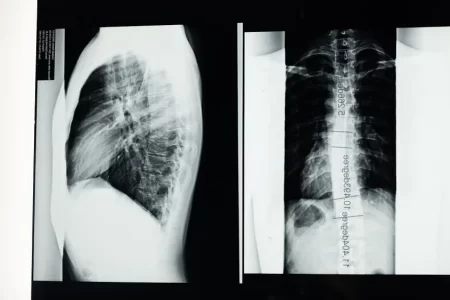
X-rays for spinal stenosis
X-rays are passed through the body in small amounts to obtain black and white images of the affected area. Any changes (for example bone spur) that occur in the back might lead to the narrowing of the space within the spinal canal which can be detected by X-ray scans.
Magnetic resonance imaging (MRI) for spinal stenosis
Powerful magnets and radio waves are used to produce cross-sectional images of the spine. MRI scans are beneficial in detecting any damage to the disks and ligaments, as well as the presence of tumors.
MRI scans show more structures, including nerves, muscles, etc compared to x-rays or CT scans. MRI scans can provide important information. For example, it can show exact pressure points on the nerves in the spinal cord.
CT myelogram
Computerized tomography (CT) scan combines with X-rays where radiations are projected at many different angles to provide detailed and cross-sectional images of the body. During a CT (computer tomography) myelogram, a spinal tap is performed in the lower back. Then, X-Ray scan followed by a CT scan is done (of the spine) to detect the narrowing of the spinal canal. This is very useful in case of lateral recess stenosis. It is also relevant for patients with implanted pacemakers where MRI is contraindicated.
In a CT myelogram, the CT scan is conducted after injecting a contrast dye into the spinal fluid. The dye outlines the spinal cord and nerves, and also reveals herniated disks, bone spurs and bone tumors.
Treatment of spinal stenosis
Treatment for spinal stenosis (narrowing of the spine) depends on the location of the stenosis and the severity of your signs and symptoms:
Physical therapy
People who suffer with spinal stenosis tend to become less active in an effort to reduce pain. This can lead to muscle weakness and more pain in later stages. Physical therapy and certain exercises may help in reducing pain. Other benefits of physical therapy are:
- Building up the strength and endurance
- Maintaining the flexibility and stability of spine
- Improving the balance
Medications
Medicines such as acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs) relieve pain and reduce inflammation. Cortisone injections into spinal column can reduce the swelling.
Pain relievers
Pain relieving medications such as ibuprofen (Advil, Motrin IB, others), naproxen (Aleve, others) and acetaminophen (Tylenol, others) can be taken on a temporary basis to ease the discomfort due to spinal stenosis. Pain relievers are typically recommended for a short period only due to lack of evidence of benefit of long-term use.
Antidepressants
Several antidepressants (tricyclic antidepressants) are given as night doses to ease the chronic pain in the spine, for example amitriptyline.
Anti-seizure drugs
Anti-seizure drugs, such as gabapentin (Neurontin) and pregabalin (Lyrica), reduces the pain caused by damaged nerves.
Opioids
Opiate is an alkaloid component of the opium poppy plant which is psychoactive. Within the plant there are some specific compounds that include morphine, thebaine, and codeine. Opoids are considered cautiously for long-term treatment. These drugs carry the risk of some serious side effects, such as “habit forming”. Drugs which are composed of codeine are considered useful for short-term pain relief. A few examples of codeine-related drugs are oxycodone (Oxycontin, Roxicodone) and hydrocodone (Norco, Vicodin).
Alternative medicine and therapy for spinal stenosis
Alternative therapies and integrated medicines are used with conventional treatments to cope with spinal stenosis pain. Examples of these alternate therapies include:
- Massage therapy
- Chiropractic treatment
- Acupuncture
Steroid injections
Nerve roots may sometimes become irritated and swollen as they are pinched in the affected area. Inflammation can be reduced by injecting a steroid medication (corticosteroid) into the space around impingement. Although it does not cure stenosis, but it can provide some relief from the pain.
Steroid injections may not be beneficial in every case and regular usage of steroid injections weakens the nearby bones and connective tissues. It is suggested that these injections can be given only a few (twice or thrice) times a year.
Surgery for spinal stenosis
Surgery should always be considered as the last option for spinal stenosis treatment. The main aim of performing a surgery for spinal stenosis is to relieve the pressure on the spinal cord or on the nerve roots by creating spaces inside the spinal canal.
Surgery is the most effective way to resolve the symptoms of spinal stenosis by decompressing the affected area. Spine surgeries have fewer complications and 80% of the affected people benefit through surgery.
Surgical procedures which are used to treat spinal stenosis include:
Interlaminar implant
A non-fusion U-shaped device is placed between two bones in the lower back which is known as interlaminar implant. It maintains the motion in the spine and keeps the spine stable after a lumbar decompressive surgery. The U-shaped device helps in retaining the height between the bones in the spine so that the nerves can exit freely and can extend to lower extremities.
Laminectomy
Lamina is the back part of the vertebrae which is affected and is removed in laminectomy. It is sometimes referred as decompression surgery. Laminectomy is the most common surgical procedure for spinal stenosis. In this procedure, some extra space is created down the nerves that put pressure on the nerves.
Sometimes, the strength of spine can be maintained by inserting a metallic link between two adjoining vertebrae. This can also be done with the help of a bone graft.
Decompression procedure
The decompression procedure is only applicable for patients with lumbar spinal stenosis and thickened ligament. To improve the spinal canal space and to remove nerve root impingement, a needle-like instrument is used. The instrument removes a small portion of a thickened ligament in the back of the spinal column to create the spinal space.
Decompression procedure is known by a few more names such as percutaneous image-guided lumbar decompression (PILD) or minimally invasive lumbar decompression (MILD).
Minimally invasive surgery
The bones or the lamina is removed in a way that causes minimum damage to nearby healthy tissue. Therefore, fusions are not mandatory after this surgery.
Fusions are a useful way to stabilize the spine and to reduce pain but by avoiding them the chances of some potential risks are also reduced. The potential risks can be post-surgical pain, swelling or inflammation and any disease in nearby sections of the spine. With reduced need for spinal fusion, minimally invasive approach to surgery shows potent result in a shorter recovery time.
The space-creating operations help to reduce spinal stenosis symptoms in most of the cases. Surgical risks during minimal invasive surgery include neurological deterioration, a tear in the membrane that covers the spinal cord, a blood clot in a leg vein or any infection.
Laminotomy
During Laminotomy, only a portion of the lamina is removed by creating a hole which is big enough to relieve the pressure at a particular spot.
Laminoplasty
Laminoplasty is performed only for cervical spine or the hinge of the neck. An opening within the spinal canal creates a hinge. Metallic hardwares bridge the gap in the opened section of the spine.
Potential future treatments for spinal stenosis
Some clinical trials are under process such as the use of stem cells to treat degenerative spinal disease. This approach is sometimes called regenerative medicine. Some trials on genomic medicine are also going on which may find applications in the treatment of spinal stenosis.
Home remedies for spinal stenosis
- Pain relievers: Over-the-counter medications such as aspirin, ibuprofen (Advil, Motrin IB, others), naproxen (Aleve, others) and acetaminophen (Tylenol, others) can help in reducing pain to some extent and also reduce the swelling or inflammation.
- Applying hot or cold packs: Applying heat or ice to the neck can help in relieving symptoms of cervical spinal stenosis.
- Maintaining a healthy weight: For a person who is obese, reducing weight can lower down the pressure or stress on the spine and it also keeps a person fit and healthy.
- Exercising: Exercises such as flexing, stretching and strengthening help in relieving the stress and opens up the spine relieving the pain. Bending the spine also becomes possible after proper exercising.
Prognosis for spinal stenosis
Most people suffering with spinal stenosis live long and remain active. Therefore, the prognosis for spinal stenosis is considered very good. People need to make modifications in their physical activities accordingly.
In some cases of severe stenosis, non-surgical treatments are not very effective and surgery may be the only feasible option. Only in very few cases, arthritis of the spine can be progressive leading to the development of new symptoms even years after surgery.
Can you prevent spinal stenosis?
Spinal stenosis cannot be prevented because it mostly occurs due to degenerative arthritis (which is associated with normal aging process). Individuals can however control the symptoms through physical therapies and exercises by keeping the bones fit and healthy. One can practice certain habits to extend the health of back and reduce its severity. These may include exercises and nutrition-rich foods.