VTE (Venous Thromboembolism): Symptoms, Causes, Diagnosis, Treatment
- Updated on: Jul 9, 2024
- 6 min Read
By
- Published on Oct 2, 2019
What is VTE (Venous Thromboembolism)?
The ability of the blood to clot is what keeps us alive. Without this ability, a simple paper cut can become an emergency. But when this blood clot affects the vein, it becomes deadly.
Venous thromboembolism (VTE) is a condition that encompasses two other conditions which are inter-related and belongs to the same spectrum. These two conditions are:
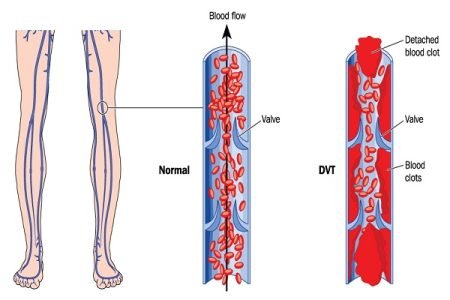
Deep vein thrombosis (DVT)
DVT is a condition in which a blood clot forms in a deep vein particularly in the leg. This can cut off the flow of the blood.
Pulmonary embolism (PE)
PE refers to a blood clot in the lungs. Pulmonary embolism occurs when a blood clot of DVT breaks free from a vein wall and travels in the circulation to the lungs. And finally it blocks the blood supply to the lungs. This condition can often become fatal.
DVT and PE when occur together are known as VTE which is actually a very dangerous and potentially deadly medical condition.
What are the symptoms of venous thromboembolism?
VTE can occur without any warning signs or symptoms. It can even go unrecognized and undiagnosed for a time period. Symptoms that appear are associated with either DVT or PE.
Signs and symptoms of the venous thromboembolism include the following:
- Onset of dyspnea (difficult or labored breathing, shortness of breath)
- Chest pain and hemoptysis (a cough that contains blood or blood-stained mucus)
- Syncope (sudden drop in heart rate and blood pressure leading to fainting)
- Sense of apprehension and anxiety
- Tachypnea (abnormally rapid breathing)
- Tachycardia (heart beats faster than normal while at rest)
- Accentuated second heart sound
- Fever
- Normal findings from lung examination
- Cyanosis (bluish or purplish discoloration of the skin or mucous membranes due to low oxygen saturation in the tissues near the skin surface)
What are the causes of venous thromboembolism?
Venous thromboembolism is caused mainly by a combination of venous stasis and hypercoagulability.
Venous stasis is responsible for forming blood clots in veins. Venous stasis is caused by long periods of immobility due to driving, flying, bed rest, hospitalization etc.
Hypercoagulability is an abnormality of blood coagulation that increases the formation of blood clots in blood vessels.
What increases the risk of venous thromboembolism?
When the flow of the blood slows down or changes, DVT occurs in the leg. The most common triggers for the condition include:
Medical treatments
There are three medical related factors that increase the likelihood of getting VTE:
- Being in the hospital for a while
- Getting a surgery (especially on the knees or hips)
- Having cancer treatments like chemotherapy
Health conditions
Certain health conditions eventually lead to VTE which include:
- Cancer (most particularly pancreatic cancer)
- Immune problems like lupus
- Certain health conditions that make the blood thicker
- Obesity
- HIV
Medications
Certain medications also increase the susceptibility to VTE:
- Hormonal replacement therapy
- Birth control pills
Other factors
Apart from the above-listed factors, there are some other things which increase the risk of VTE:
- Earlier episode of VTE
- Staying in the same position for a long time
- Family history of blood clots
- Excess smoke
- Pregnancy and the postpartum period
- Age above 60 years
How is venous thromboembolism diagnosed?
There is no blood test that can accurately diagnose deep vein thrombosis. A variety of imaging tests are used to confirm the diagnosis. The tests include:
Doppler ultrasound
In this procedure, high-frequency sound waves are used to visualize large veins and detect a clot if there is any in the vein. This method is most commonly used because it is painless and does not involve any complications. However, a clot in the smaller veins can sometimes be missed in this method.
Venography
Suspected veins are injected with a liquid dye for imaging studies. The dye highlights blockage of blood flow by a clot. This is the most accurate test but rarely used in today’s time because of the availability of improved ultrasound technology.
Impedance plethysmography
Any volume changes within veins can be detected by this test by using electrodes. It is rarely used these days because it does not work better than ultrasound and is harder to perform.
CT scan
CT scan provides a very detailed look of the leg veins in cross section. Blood clots can be easily detected using this technique. CT scan is used mainly in the identification of blood clots in the lungs.
How is venous thromboembolism treated?
Venous thromboembolism is a dreadful condition and needs to be treated right after the diagnosis results are positive. The different methods of treatment include:
Anticoagulation
Anticoagulant medicines are used to prevent blood clots getting bigger. They can also help to stop the blood clot from breaking off and lodging to another part of the bloodstream. These medicines mainly alter the proteins present in the blood and prevent clot forming so easily. There are various types of anticoagulants that are used to treat DVT.
Heparin
Heparin is available in two different forms. First one is standard (unfractioned) heparin which is given as:
- an intravenous injection (straight into veins)
- an intravenous infusion (a continuous drip of heparin is fed through a narrow tube into a vein in the arm)
- a subcutaneous injection (injection under the skin)
The second form of heparin is low molecular weight heparin (LMWH) which is usually given as a subcutaneous injection. The effects of LMWH are more reliable than standard heparin.
Side effects of heparin include:
- a skin rash and other allergic reactions
- bleeding
- weakening of the bones if taken for a long time
Warfarin
Warfarin is taken as a tablet after initial treatment to prevent further blood clots occurring. It is recommended for about three to six months. Sometimes, it may be taken for a longer period as the doctor suggests. If the patient is taking warfarin, he or she should:
- keep the diet consistent
- limit the amount of alcohol
- take warfarin at the same time every day
- not start any other medicine without checking with the doctor
- not take herbal medicines
Rivaroxaban
Rivaroxaban is a medication that helps prevent recurrent DVT and pulmonary embolism. It comes in tablet form. It inhibits a substance called factor Xa and restrict the formation of thrombin (an enzyme that helps blood clot) thus preventing the formation of blood clots.
Apixaban
Apixaban is used in the treatment and prevention of DVT and pulmonary embolism. It is taken orally as a tablet. It also prevents blood clots formation by hindering factor Xa and restricting the formation of thrombin.
Exercise
Exercise is the key to every problem. And in the case of VTE too, it is helpful. Doctors usually advise patients to walk regularly. This can help prevent symptoms and may help to prevent the complications of DVT.
Raising the leg
Raising the leg while resting helps to relieve the pressure in veins. It also stops blood and fluid pooling in the calf. Slightly raising the end of the bed also ensures that the foot and calf are slightly higher than the hip.
Inferior vena cava filters
Inferior vena cava (IVC) filters are also used as an alternative to anticoagulant medicines when anticoagulant treatment does not work. These filters are small vascular devices that can be implanted in a vein. The main work of the filter is to trap large fragments of a blood clot and prevent them to travel to the heart and lungs.
Inferior vena cava filters can be placed in the vein permanently or temporarily and can be removed after the risk of a blood clot has decreased.
How to prevent venous thromboembolism?
The goal of VTE treatment is to shrink the clot and prevent other clots from forming. The doctor can give certain tips on preventing VTE, which might include:
- Avoiding long periods of sitting. While travelling by plane or car, taking a break and walking every hour is good to keep the blood flowing in the legs.
- When seated, avoid crossed legs as they interfere in the blood flow.
- Obesity increases the risk for DVT. Try to reduce the extra weight and maintain a healthy weight.
- Focus on healthy and balanced diet.
- Staying active can prevent blood clots from forming. Therefore move around and indulge in some form of exercise.
- Quit smoking and drinking.
What are the complications of venous thromboembolism?
The complications associated with venous thromboembolism are:
Pulmonary embolism
A pulmonary embolism occurs when a blood clot from another part of the body (usually leg) travels to the lung and block the blood vessel in the lung. This condition can be life-threatening. It’s important to identify the signs and symptoms of a pulmonary embolism and seek urgent medical attention.
Signs and symptoms of a pulmonary embolism include:
- Sudden shortness of breath
- Chest pain or discomfort that worsens while deep breathing and coughing
- Feeling lightheaded, dizzy or fainting
- Rapid pulse
- Coughing up blood
Postphlebitic syndrome
This condition occurs as an after effect of deep vein thrombosis which can damage the veins when the blood clot reduces blood flow in the affected areas.
The symptoms of the postphlebitic syndrome are:
- Persistent swelling of the legs
- Leg pain
- Skin discoloration
- Skin sores