What Are the Chances of Surviving Endocarditis?
- Updated on: Aug 1, 2024
- 4 min Read
- Published on Feb 4, 2020
Endocarditis
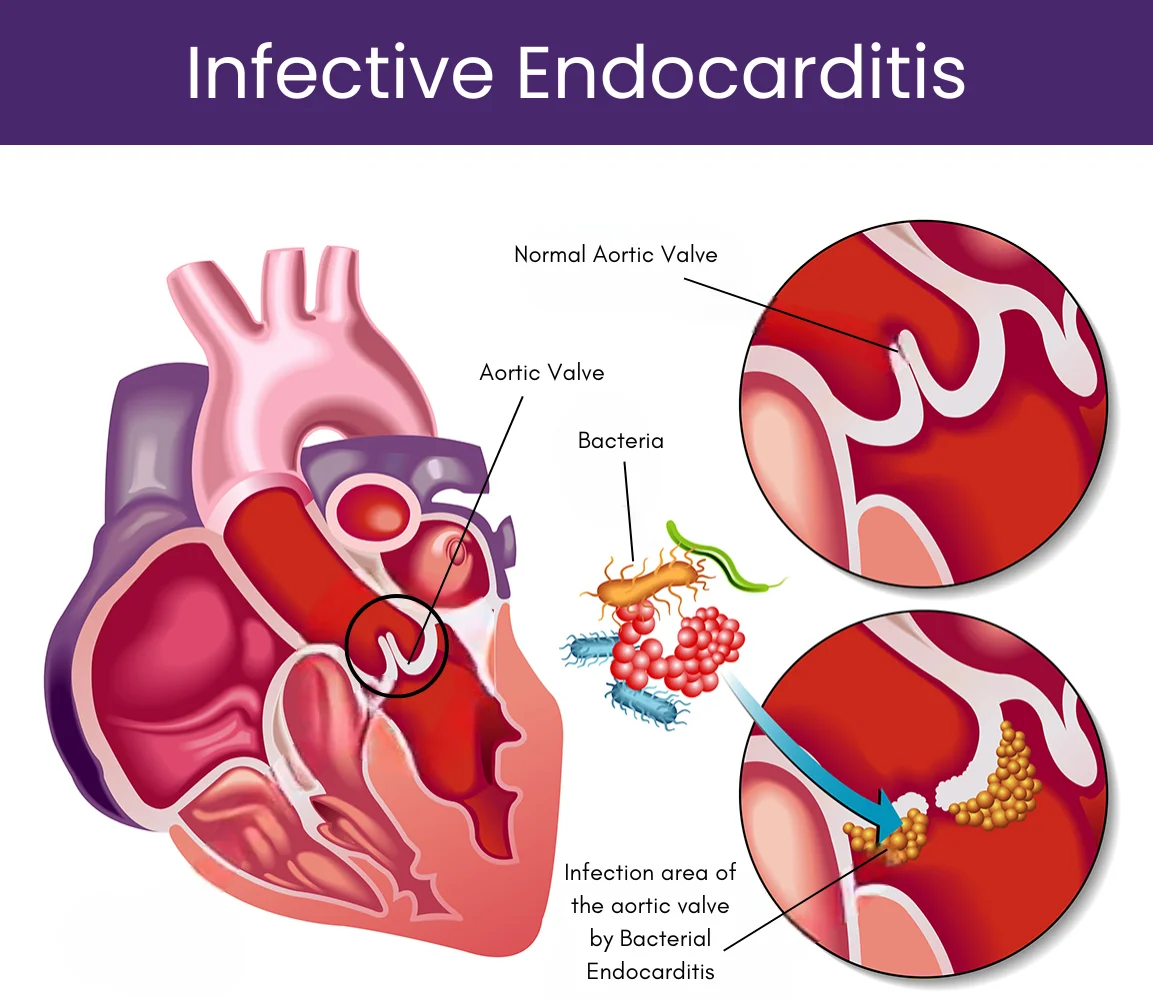
Endocarditis or infective endocarditis is an inflammation of the heart valves and endocardium (inner lining of the heart chambers) due to infections caused by some infectious organisms like bacteria or fungi. These infectious organisms can enter the bloodstream and settle within the heart. In most cases, these organisms are streptococci (“strep”), staphylococci (“staph”) or species of bacteria that normally reside on our body surfaces. These infectious organisms get entry into our bloodstream through skin cuts and injuries, dental or medical procedures, skin disorders, or skin pricks (in case of intravenous drug users).
Overgrowth of bacteria is one of the main causes of endocarditis. These bacteria normally reside on our inner and outer body surfaces but we can give them entry into our blood stream by eating or drinking. Normally our immune system protects us from such infectious encounters by fighting off germs but this process fails in some people with compromised immune functions.
In people with infective endocarditis, the germs travel through their bloodstream and then enter into the heart, where they multiply in large numbers and ultimately lead to the inflammation. Besides bacteria, endocarditis can also be caused by fungi or other germs.
There are many signs and symptoms of endocarditis. Some of them may include:
- High body temperature (over 100 degrees)
- Night sweats
- Rashes on Skin
- Pain, tenderness, redness or swelling
- Unhealed wound or cuts
- Warm, red, draining sores
- Sore and scratchy throat
- Sinus drainage
- Nasal congestion
- Persistent cough
- Presence of white spots on your mouth and tongue
Prognosis or Outlook of Endocarditis
Despite various diagnostic and therapeutic procedures, infective endocarditis is associated with high mortality and serious complications. Assessing the prognosis of endocarditis for patients involves the differentiation of three clinical procedures –
(a) Prognostic assessment at admission
(b) Early risk reassessment during the first week of antibiotics, and
(c) Short- and long-term prognosis after discharge
These are the three important parameters for diagnosis and prognosis of endocarditis patients. These parameters are based on physical examination of patients like heart failure signs, echocardiography for checking periannular complications, and blood cultures for detecting S. aureus infections.
If left untreated, infective endocarditis can be fatal. After treatment, the death risk depends on various factors like age of a person, infection duration, the presence of a replacement heart valve, causative organism, and the amount of damage done to the heart valves. Nevertheless, with an appropriate antibiotic treatment, most people can survive.
With the help of a proper diagnosis and medical treatment, more than 90 percent of patients suffering from bacterial endocarditis can recover. It has been found that those patients who have endocarditis in right side of their heart usually have a better outlook than those with left-side endocarditis. In some cases, it has been found that endocarditis caused by fungi, has a low prognosis when compared with bacterial endocarditis.
There are various serious complications of endocarditis such as congestive heart failure, emboli (floating blood clots) that can enter into our brain, lungs or coronary arteries, and kidney complications. Untreated acute endocarditis can be risky in less than 6 weeks. Without treatment, subacute endocarditis can cause death within 6 weeks to one year.
Infective endocarditis (IE) being a serious disease has an elevated short- and long-term mortality. There is a poor prognosis for IE not only due to the high in-hospital mortality rate and high in-hospital mortality complications but also due to late sequelae that appear once the infection is over.
Recent progresses in diagnostic techniques and antibiotic treatment has improved the short-term prognosis for infective endocarditis (IE) due to prior detection of complications.
Role of Surgery in the Prognosis of Infective Endocarditis
Infective endocarditis is one of the deadly diseases associated with an in-hospital mortality rate of 10–30%. Among them, 50% required cardiac surgery in their acute phase. The two main objectives of heart surgery in such patients mainly involve complete removal of the infected tissue and renewal of cardiac morphology, including repair or replacement of the affected valves. During the operation, different types of valves such as a biological valve, mechanical valve, autograft and homograft may be used as required.
According to The 2014 American College of Cardiology/American Heart Association(ACC/AHA) guidelines, a biological valve is recommended in patients of 65 years age or older, while a mechanical valve is appropriate for patients under 65 years of age, but there are no specific guidelines or recommendations for surgery of infective endocarditis.
It has been suggested that mechanical valves provide a considerably better prognosis in infective endocarditis patients. Moreover, there were considerable differences in the clinical features of patients with biological valve compared to patients receiving a mechanical valve. A study suggested that any mortality risk of the biological valve group patients was significantly higher than that of the mechanical valve group patients.
Can Valvular Surgery Decrease Mortality Rates in Endocarditis Patients?
According to an investigation published in the November 23/30 issue of JAMA, it has been suggested that approximately two-thirds of patients with heart failure and infective endocarditis require valvular surgery, which has been associated with a substantial reduction in the risk of mortality in hospital and one year after the surgery.
Some prior studies have suggested that the risk of mortality due to infective endocarditis and heart failure can be decreased with the help of valvular surgery. The procedure has been strongly recommended by the American College of Cardiology/American Heart Association and European Society of Cardiology.
Researchers have found that patients who have undergone a valvular surgery had a very low mortality rate as compared to patients who had received medical treatment only. Mortality rate of patients with valvular surgery was found to be 20.6 percent and mortality rate was found to be 44.8 percent in patients who were on medical treatment only. Furthermore, the researchers observed that valvular surgery patients had a one-year mortality rate of 29.1% compared to 58.4% in patients with only medical therapy.












9 Comments
This is sensible info! Where else will if ind out more?? Who runs this joint too? sustain the good work
You have mentioned very interesting details ! ps decent web site .
I think other website proprietors should take this internet site as an example , very clean and fantastic user genial style .
Perhaps you should also a put a forum site on your blog to increase reader interaction.~”~~~
I wish I had a dime for every bad article I’ve read lately. I also wish other writers had your talent and style. Thank you.
But I see that the original post was published more than two years ago. Was there are any update for this elsewhere on the page?
Needed to send you this little remark to help give many thanks over again for all the remarkable knowledge you have shown here. It was certainly pretty generous of people like you in giving openly exactly what some people would have offered as an e-book to earn some dough for their own end, principally since you might well have done it if you considered necessary. The creative ideas as well acted to become a fantastic way to fully grasp the rest have a similar dreams just like mine to realize great deal more with reference to this matter. I am certain there are some more enjoyable situations in the future for individuals who see your site.
I’m new to your blog and i really appreciate the nice posts and great layout.*,”-’
It’s exhausting to find educated people on this topic, however you sound like you recognize what you’re speaking about! Thanks