What is Non-Gonococcal Urethritis (NGU)?
- Updated on: Jul 13, 2024
- 5 min Read
By
- Published on Oct 3, 2019


What is non-gonococcal urethritis?
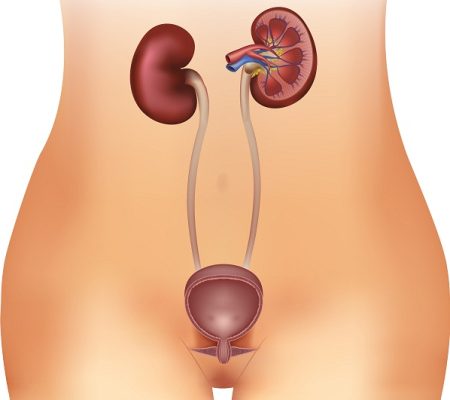
Urethritis refers to an inflammation that affects the urethra (the tube that carries urine from the bladder out of the body).
Usually, an infection is the main cause of the inflammation. When the condition is caused by pathogens (germs) and not by the sexually transmitted infection gonorrhea, it is known as non-gonococcal urethritis (NGU). Sometimes, it is called non-specific urethritis (NSU) when no cause can be found.
Urethritis is the most common condition and is a sexually transmitted disease. Read about urithritis in general.
Who gets non-gonococcal urethritis?
NGU is commonly found in men because the organisms that cause this infection are sexually transmitted and the male urethra is always at higher risk of infection during intercourse (female urethra is seldom infected during intercourse).
Teenage boys and men in their twenties, having multiple sex partners are most at risk for this type of infection.
How common is non-gonococcal urethritis?
Several types of organisms can cause NGU. The most common and serious of them is chlamydia. Chlamydia is common in both males and females. But, due to anatomical differences, the diagnosis of NGU is more commonly made in males than in females.
Some of the germs that can cause NGU include:
- Chlamydia trachomatis (most common)
- Ureaplasma urealyticum
- Trichomonas vaginalis (rare)
- Herpes simplex virus (rare)
- Haemophilus vaginalis
- Mycoplasma genitalium
How is non-gonococcal urethritis transmitted?
Non-gonococcal urethritis is transmitted by three ways which include:
Sexual
- Most of the germs responsible for NGU are passed during intercourse (that may be vaginal, anal or oral) as it involves direct mucous membrane contact with an infected person.
- These germs can be passed even if body fluids are not exchanged.
Nonsexual
- Urinary tract infections
- Bacterial prostatitis (an inflamed prostate gland due to bacteria).
- Urethral stricture (a narrowing or closing of the tube in the penis).
- Phimosa (a tightening of the foreskin of the penis that makes it hard to pull back).
- Catheterization (any process that may involve inserting a tube into the penis).
Perinatal
During birth, infants are at high risk as they are exposed to the germs causing NGU in passage through the birth canal. This may cause the infections in such as:
- eyes (conjunctivitis)
- ears
- lungs (pneumonia)
What are the symptoms of non-gonococcal urethritis?
The symptoms are seen or experienced more in the morning and are given below:
Men (urethral infection)
- Heavy discharge from the penis
- Burning sensation or pain when urinating
- Itching, irritation, discomfort or tenderness
- Underwear stains
Women (vaginal/urethral infection)
Sometimes women may also be asymptomatic (have no symptoms). Symptoms of NGU in women can include:
- Creamy to white discharge from the vagina
- Burning sensation or pain when urinating (peeing)
- Abdominal pain
- Heavy vaginal bleeding (when infection has progressed to pelvic inflammatory disease (PID))
Anal or Oral Infections
Anal infection may result in:
- Rectal itching
- Discharge
- Pain on defecation
Nearly, 90 percent of the oral infections are asymptomatic (have no symptoms), but some people might have a sore throat.
What are the causes of non-gonococcal urethritis?
Most common causes of non-gonococcal urethritis include an infection, irritation or damage to the urethra. There are also many cases where no cause is found as such.
Causes of non-gonococcal urethritis include:
Sexually transmitted infections (STIs)
Chlamydia is one of the most common sexually transmitted infections that cause non-gonococcal urethritis. Chlamydia is spread through unprotected sex (sex without a condom), anal and oral sex.
Urethritis is more common among people who are at a risk of sexually transmitted infections. Such people include:
- Sexually active people
- Those have had unprotected sex
- People with multiple sexual partners
Other infections
A number of other infections can cause NGU involving bacteria that usually live harmlessly in the throat, mouth or rectum. These bacteria if get into the urethra can cause NGU such as during oral or anal sex. Infections that can cause NGU include:
Trichomonas vaginalis
It is an infection that is caused by a tiny parasite.
Mycoplasma genitalium
It is caused by a pathogenic bacterium that lives on the ciliated epithelial cells of the urinary and genital tracts in humans.
Urinary tract infection
It is an infection in any part of the urinary system, the kidneys, bladder or urethra.
Herpes simplex virus
This is responsible for most cold sores and genital herpes.
Adenovirus
This usually causes a sore throat or an eye infection.
Non-infectious causes
Non-gonococcal urethritis can be caused by non-infectious causes when something else leads to the urethra becoming inflamed. Non-infectious causes of NGU include:
- Irritation and inflammation caused by products used in the genital area such as soap, deodorant, body wash or spermicide.
- Damage to the urethra caused by vigorous sex or masturbation.
- Damage to the urethra caused when catheter is inserted during an operation.
How is non-gonococcal urethritis diagnosed?
In order to diagnose non-gonococcal urethritis, two tests can be done. Both tests are carried out to ensure the diagnosis is correct. The tests are:
Swab test
This test is conducted using a swab. A swab is like a small cotton bud which has a plastic loop at the end. With the help of swab, a sample of fluid is taken from your urethra. This test is not painful but the patient may feel a little uncomfortable for a few seconds.
Urine test
A sample of patient’s urine is taken and is tested for the infection. This test provides more reliable results. The patient is asked not to urinate for at least one hour before providing a urine sample.
What are the treatment options for non-gonococcal urethritis?
There are various steps in the treatment of non-gonococcal urethritis. Each step is to be followed with proper care and attention to prevent the infection coming back.
Antibiotics
Antibiotics may be prescribed to the patient even before he receives his test results. Most commonly prescribed antibiotic tablets or capsules are:
- Azithromycin 1 g orally in a single dose
- Doxycycline 100 mg orally twice a day for 7 days
Some of the alternative antibiotics that can be given are:
- Erythromycin base 500 mg orally four times a day for 7 days
- Erythromycin ethylsuccinate 800 mg orally four times a day for 7 days
- Levofloxacin 500 mg orally once daily for 7 days
- Ofloxacin 300 mg orally twice a day for 7 days
For recurrent and persistent urethritis, following antibiotics are prescribed:
- Metronidazole 2 g orally in a single dose with azithromycin 1 g orally in a single dose (if not used for initial episode)
- Tinidazole 2 g orally in a single dose with azithromycin 1 g orally in a single dose (if not used for initial episode)
Some of the side effects of antibiotics include feeling sick, vomiting and diarrhea.
Follow-up
- Take all medications even if you start to feel better before you finish the bottle.
- Inform all partners.
- Treat all partners.
- Treat gonorrhea if the tests indicate the infection.
- Abstain from sex until treatment is completed.
How can non-gonococcal urethritis be prevented?
Non-gonococcal urethritis can be prevented by following certain things which are given below:
- Abstain from sex until the treatment is completed.
- Using latex condoms every time you have sexual intercourse.
- Practice mutual monogamy which means having sex with only one uninfected partner.
- For additional protection, water-based spermicides can be used along with latex condoms.
- Carefully wash genitals after sexual relations.
- Have regular check-ups if you are sexually active.
- Always seek qualified and prompt medical intervention.
- Know your partner because careful consideration and open communication between partners may protect from infection.
What are the complications of non-gonococcal urethritis?
For men, complications may include:
- Epididymitis (inflammation of the epididymis which are structures along the posterior border of the testes).
- Reiter’s syndrome (arthritis)
- Conjunctivitis
- Skin Lesions
- Discharge
For women, complications are:
- Pelvic Inflammatory Disease (PID) which can result in ectopic (tubal) pregnancy.
- Recurrent PID which may lead to infertility.
- Chronic pelvic pain
- Vaginitis
- Mucopurulent cervicitis (MPC)
- Spontaneous abortion
Serious complications can also occur though they are rare. These may include, such as:
Reactive arthritis: The immune system attacks healthy tissues. This leads to joint pain and conjunctivitis.
Epididymo-orchitis : Inflammation inside the testicles