Vomiting Blood (Haematemesis): Why Do People Throw Up Blood?
- Updated on: Jun 11, 2024
- 10 min Read
- Published on Apr 21, 2021

Vomiting Blood (Hematemesis)
Vomiting blood, also called hematemesis, is the puking up of stomach contents along with blood, or throwing of the blood only. Vomiting blood can be a scary and a discomforting experience for many people. In some cases, blood transfusions may be necessary to help replenish blood volume and restore health.
Throwing up the blood either mixed with or without stomach contents could be a sign of a serious problem such as internal injuries, organ bleeding, or organ rupture. In some cases, it could be due to a minor cause such as swallowing blood from a mouth injury or from a nosebleed. Such minor causes usually do not cause any long-term harm.
When experiencing the scary sight of vomiting blood, it’s important to act fast in stopping the bleeding. Haematemesis can occur due to a variety of reasons, including severe gastrointestinal issues, liver disease, or even excessive alcohol consumption. Seeking medical attention is crucial to not only identify the cause but to prevent any further complications. In some cases, immediate treatment may be necessary to stop the bleeding and ensure a full recovery. Don’t hesitate to get help if you or someone you know is experiencing this concerning symptom. Stopping the bleeding is the first step to finding the root of the problem and getting back to good health.
Types of Vomited Blood: How Does the Vomited Blood Look Like?
Regurgitated blood may look brown, black, bright red, or dark red in color. Brown blood generally resembles coffee grounds when vomited, called coffee ground blood.
The color of your vomited blood can indicate the source and severity of the bleeding in your organs. For example, darker blood often occurs due to the bleeding from an upper gastrointestinal (GI) source, such as the stomach. Bright red blood is generally indicative of severe bleeding from the esophagus or stomach. The color of blood in the vomit does not always indicate the source and severity of the bleeding, but it helps the doctor to start investigation.
The amount and colour of the blood in vomit can also vary:
- vomiting large amounts of bright red blood
- only streaks of blood in the vomit, mixed up with stomach contents such as food
- small pieces of blood clots, something similar to coffee grounds in the vomit
If you vomit large amounts of blood, about the size of a small cup, or if you experience dizziness or changes in breathing after the vomiting, you should call emergency immediately. This might require an urgent medical attention.
More: Blood in urine (Hematuria)
Common Causes of Vomiting Blood: Why Am I Vomiting Blood?
The most common causes of vomiting blood are listed here. They may range in severity from minor to major. It’s a basic guide to give you an idea of the problem. However, you shouldn’t use it to diagnose the condition by yourself. You must contact an expert for the diagnosis and emergency treatment.
Minor Conditions Causing Vomiting Of The Blood
- swallowing of the blood
- swallowed foreign object that causes problem inside the body
- tear in the esophagus due to coughing
- Vigorous vomiting
- esophagus irritation
- nosebleeds
Serious Causes Of Vomiting Blood
- alcoholic hepatitis
- erosion of the stomach lining
- pancreatic cancer
- liver cirrhosis
- esophageal cancer
- swallowing of poisons, such as corrosive acids or arsenic
Other Common Causes Of Vomiting Blood
- side effects of non-steroidal anti-inflammatory drug
- pancreatitis
- aspirin side effects
- gastritis (stomach inflammation)
- a blood condition, such as a reduced number of platelets in the blood, leukaemia, haemophilia or anaemia
- severe gastro-oesophageal reflux disease (GERD)
- esophageal varices
Vomiting Of The Blood In Infants And Young Children Can Be Caused Many Other Conditions Such As:
- Lack of vitamin K
- Milk allergy
- Blood clotting problems
- Swallowed blood or a swallowed foreign object
- Birth defects and abnormalities
Some major causes of the vomited blood (Haematemesis) are discussed here.
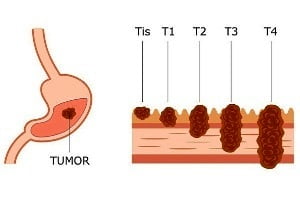
Vomiting Blood As A Sign Of Colon Cancer Or Colorectal Cancer
Many cases of colorectal cancer have no symptoms or warning signs until the cancer has advanced. Vomiting can be one of these signs. However, it is important to note that vomiting can be caused by a number of other normal problems such motion sickness, unpleasant sights or smells.
If nausea and vomiting are accompanied with other symptoms such as constipation or pain, colon cancer could be the cause. When vomiting is a symptom of colon cancer, it is usually because a tumor is causing a bowel obstruction. Vomiting may be accompanied with blood depending on the severity of the blockage. With colon cancer, some patients throw up blood quite frequently. But it is usually accompanied with other conditions such as abdominal pain, changed bowel movements, constipation, etc.
Gastro-Esophageal Reflux Disease (GORD)
Gastro-esophageal reflux disease (GORD or GERD) occurs when acid leaks out of the stomach and enter into the esophagus. Acid reflux occurs when sphincter muscles at the lower section of the esophagus relaxes at the wrong time, allowing stomach acid to move up into your esophagus.
Severe form of GORD can cause irritation and tear of the lining of your esophagus and start bleeding. A tear in the lining of esophagus due to prolonged irritation can also cause bleeding and blood-mixed vomiting.
Esophageal Varices And Throwing Up Blood
Esophageal varices are enlarged veins that develop in the walls of the lower section of the esophagus. They can cause bleeding. Usually, they don’t cause any pain.
Esophageal varices generally develop in liver diseases. You might be asked for admission in hospital of the suspected cause of vomiting with blood is esophageal varices.
The most serious cause of esophageal varices is cirrhosis.
Gastritis And Vomiting Blood
Gastritis is a condition characterized by inflammation of the stomach lining. Acute gastritis involves severe inflammation and usually occurs suddenly. Chronic gastritis involves long-term inflammation that can last for years if left untreated and develops gradually.
A person with gastritis may experience a burning pain in the stomach. Bleeding may occur if the inflammation causes damage to arteries in the region. Generally, gastritis is not a serious condition but it can last for years without treatment, and may ultimately cause development of ulcer or cancers in the stomach.
There are many causes of gastritis such as infection, regular use of non-steroidal anti-inflammatory painkillers, excessive use of alcohol, stress etc.
Peptic ulcers: Stomach ulcers, Duodenal ulcers
Stomach ulcers (gastric ulcers) are open sores that develop on the lining of the stomach. They can also develop in the intestine right beyond the stomach. These are called duodenal ulcers. Stomach ulcers and duodenal ulcers are together referred to as peptic ulcers.
These ulcers may cause bleeding which may also appear in the form of vomiting. Blood from a stomach ulcer or cancer may be bright red or dark brown with a grainy appearance like that of coffee grounds. It may be accompanies with a burning or gnawing sensation in the stomach travelling up to the neck and down to the belly button, or through the back.
Vomiting Blood As A Sign Of Esophageal Cancer
Vomiting blood is not the main symptoms of esophageal cancer, but it eventually affects patients suffering from this type of cancer. Usually, patients experience problems such as difficulty in swallowing, which is a common sign of the tumor or cancer in esophagus. Vomiting blood only occurs if the cancer grows rapidly. The growth of esophageal cancer is not accompanied by sufficient growth of the blood vessels that supply nutrients to the tumor. Some parts of the tumor may become necrotic and start bleeding. Bleeding of the esophageal cancer is also possible during radiation therapy of the cancer.
Bleeding from the esophagus in patients with esophageal cancer is not a good sign and may indicate to progression of the disease. People who have developed an esophagotracheal fistula may have more esophageal bleeding.
Pancreatic Cancer And Puking Blood
Sometimes, you may throw up blood due to pancreatic cancer. Pancreatic cancer begins in the tissues of your pancreas, an organ in the abdomen that lies horizontally behind the lower part of the stomach. Pancreas releases enzymes that help in digestion and hormones that help control blood sugar levels.
Nausea and vomiting occurs particularly during later stages of the pancreatic cancer, when the tumor has grown significantly large enough to block at least a part of the gastrointestinal tract (mainly the duodenum).
Blood Vomiting In Liver Cirrhosis
Varices are enlarged and swollen blood vessels in the lining of the stomach. One of the reasons why varices develop is liver cirrhosis or alcoholic liver diseases. In cirrhosis, scarred liver tissue blocks blood flow through the liver. This increases the pressure. The increased pressure pushes back into the gut and causes the veins to inflame in the stomach.
Cirrhosis is a serious condition of liver, where normal tissue is replaced by scarred tissue. The condition progress slowly and often does not cause symptoms in the beginning. With liver gradually becoming worse, serious problems start developing. Blood in vomiting can be an indication of the advanced liver disease. Read about liver cirrhosis.
Bleeding which has not come from the gut
Sometimes, vomited blood comes from somewhere else and not from the gut. If you have had a nosebleed and then swallowed the blood, you may vomit it. Sometimes, it may be blood with coughing, which is generally not a major problem. Often, it is difficult to tell whether the blood has been vomited from the gut, or coughed up.
Living With Hematemesis: Coping and Improving Quality of Life
Living with hematemesis can have a significant emotional toll on individuals, including anxiety, depression, and social isolation. It can impact patients’ quality of life and their ability to perform daily activities.
Hematemesis refers to the condition of throwing up blood, which can occur due to various underlying medical conditions such as peptic ulcers, esophageal varices, and gastrointestinal tumors. It can also result from traumatic injuries, medication side effects, and liver disease.
According to recent research studies, prompt medical attention is critical for patients experiencing hematemesis. Treatment options include blood transfusions, medication, and surgical procedures. Additionally, managing symptoms such as nausea, vomiting, and pain can be challenging for patients.
Coping With Hematemesis
Hematemesis, or vomiting blood, can be a distressing experience that requires careful management to ensure the best possible outcome for patients. For healthcare professionals, managing symptoms such as nausea and vomiting is key to improving quality of life for patients. Antiemetics, such as ondansetron or metoclopramide, can be used to control nausea and vomiting, while proton pump inhibitors or H2 receptor antagonists can help control gastric acid production.
Staying hydrated and nourished with a proper diet is also essential for patients with hematemesis. In some cases, patients may need to follow a liquid or soft food diet to prevent further bleeding or irritation. Patients should also avoid alcohol and certain medications that can irritate the stomach lining and exacerbate the condition.
Adjusting daily activities to manage the condition can also be beneficial for patients with hematemesis. Patients should avoid strenuous activities or lifting heavy objects that can put pressure on the abdominal area and potentially trigger an episode of vomiting. Stress management techniques, such as meditation or deep breathing, can also help manage anxiety and stress related to the condition.
Working with healthcare providers to manage symptoms and prevent further episodes of hematemesis is crucial for patient care. Endoscopy or imaging tests may be used to identify the underlying cause of the condition, while medication or surgical interventions may be necessary to treat the underlying condition and prevent further episodes of hematemesis.
Improving Quality of Life
Living with the condition of hematemesis, or throwing up blood, can be a challenging experience that impacts a person’s mental health and relationships. It is important for healthcare professionals to be aware of these challenges and to provide support to patients in managing their symptoms and improving their quality of life.
Understanding the Impact of Hematemesis on Mental Health and Relationships
Hematemesis can have a significant impact on a person’s mental health, leading to anxiety, depression, and feelings of isolation. It is important for healthcare professionals to be aware of these potential impacts and to provide resources and support to help patients manage these challenges.
Research studies have shown that people with hematemesis are more likely to experience anxiety and depression compared to the general population. This is thought to be related to the unpredictability of the condition, the physical symptoms associated with it, and the potential impact on a person’s quality of life.
Additionally, hematemesis can also impact a person’s relationships, leading to feelings of isolation and social withdrawal. Healthcare professionals should encourage patients to communicate openly with their loved ones about their condition and its impact on their daily life.
Coping With Anxiety and Depression
For patients with hematemesis, coping with anxiety and depression is a crucial aspect of improving their quality of life. Cognitive-behavioral therapy (CBT) is a type of therapy that has been shown to be effective in managing these conditions. It involves identifying negative thought patterns and developing strategies to manage them. Other strategies for managing anxiety and depression include practicing mindfulness meditation, regular exercise, and stress reduction techniques such as deep breathing exercises.
Building a Support System of Friends, Family, and Healthcare Providers
Building a support system of friends, family, and healthcare providers is an essential aspect of managing hematemesis. Patients should be encouraged to communicate openly with their loved ones about their condition and its impact on their daily life. They should also be connected with healthcare providers who can provide the medical care and emotional support they need.
Seeking Professional Help for Mental Health Concerns
For patients with hematemesis, seeking professional help for mental health concerns is crucial for improving their quality of life. Healthcare professionals should provide information about available mental health resources and encourage patients to seek help when needed.
Preventing Future Episodes of Hematemesis
Preventing Future Episodes of Hematemesis: Strategies for Healthcare Professionals
When a patient presents with the symptoms of throwing up blood, it is essential to identify the underlying cause to prevent future episodes. Hematemesis can be caused by various medical conditions, ranging from gastrointestinal disorders to bleeding disorders. In this article, we’ll discuss three key strategies that healthcare professionals can use to prevent future episodes of hematemesis.
Identifying the Underlying Condition Causing the Hematemesis
To prevent future episodes of hematemesis, it is essential to identify the underlying condition that is causing the bleeding. The diagnostic process may involve a range of tests, including blood tests, endoscopy, and imaging studies. The most common causes of hematemesis include peptic ulcers, gastritis, esophageal varices, and cancer. Early identification of the underlying condition can help healthcare professionals develop an effective treatment plan that can prevent future episodes of hematemesis.
Following Prescribed Treatment Plans
Once the underlying condition causing the hematemesis has been identified, healthcare professionals must develop a treatment plan that targets the root cause of the bleeding. Treatment plans may include medications, dietary modifications, and in some cases, surgery. It is essential that patients follow the prescribed treatment plan to prevent future episodes of hematemesis. Healthcare professionals should monitor patients closely to ensure that they are responding well to the treatment and make adjustments as needed.
Avoiding Triggers That May Cause Hematemesis, Such as Alcohol or Certain Medications
Certain triggers can cause or exacerbate hematemesis. These triggers may include alcohol, certain medications such as non-steroidal anti-inflammatory drugs (NSAIDs), and other substances that irritate the stomach lining. Patients should be advised to avoid these triggers to prevent future episodes of hematemesis. Healthcare professionals should provide patients with clear instructions on which substances to avoid and offer alternatives where appropriate.
FAQs
Should I go to the ER if I throw up blood?
Yes, if you throw up blood, it is important to seek medical attention immediately. It can be a sign of a serious medical condition that requires prompt evaluation and treatment.
Can vomiting blood cause death?
Yes, vomiting blood can be a sign of a life-threatening condition such as bleeding in the digestive tract, which can lead to shock and death if not treated promptly.
How to tell if there is blood in vomit?
Blood in vomit can appear bright red, dark red, or look like coffee grounds. If you suspect that there is blood in your vomit, you should seek medical attention.
Is a little blood in vomit normal?
No, any amount of blood in vomit is not normal and should be evaluated by a healthcare provider.
What are the first signs of internal bleeding?
The first signs of internal bleeding can vary depending on the location and severity of the bleeding. Common signs include pain, swelling, dizziness, weakness, nausea, vomiting, and changes in mental status. If you suspect that you have internal bleeding, seek medical attention immediately.